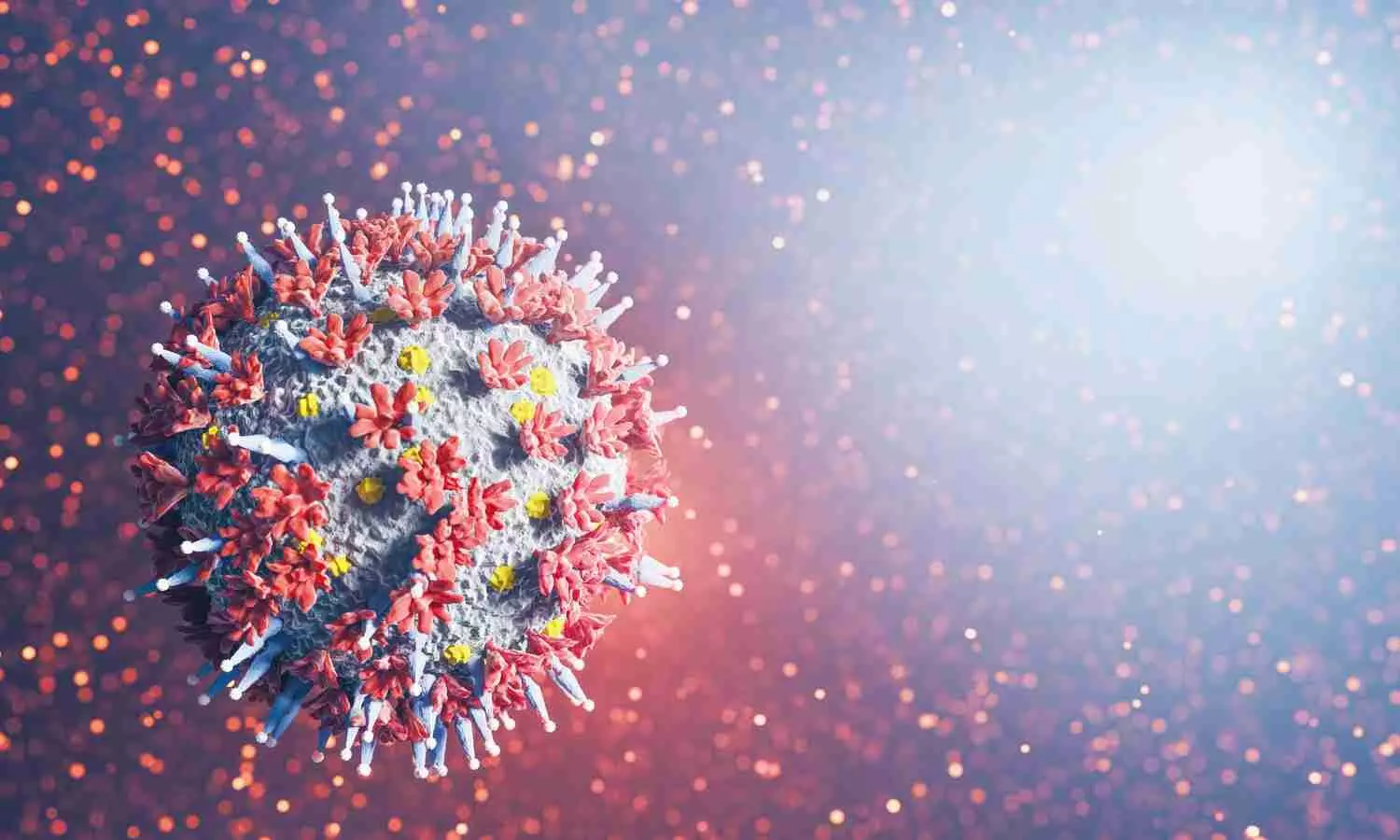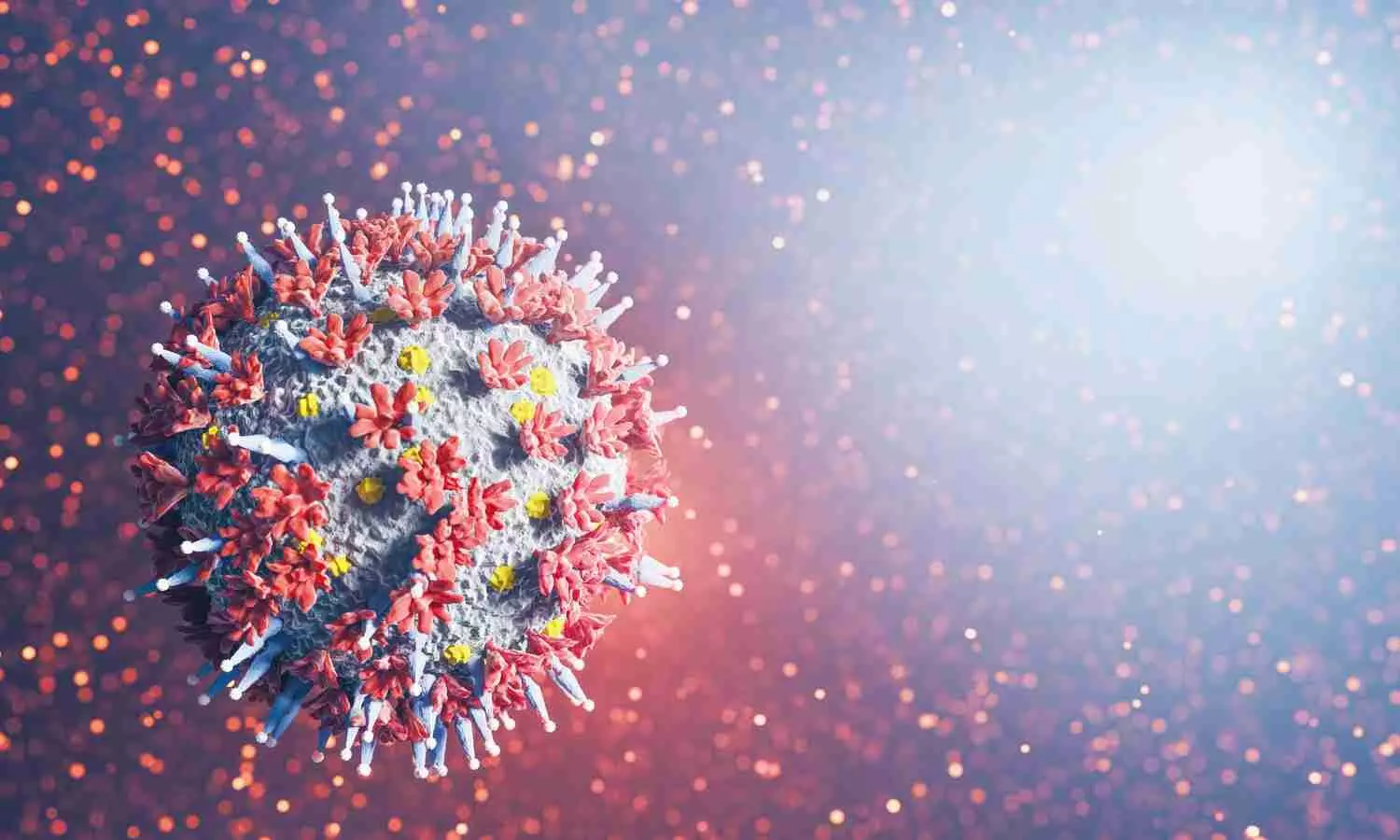
USA: A recent study has suggested that decreased circulating monocytes are associated with reduced lung function and uniquely distinguish late-resolving COVID-pulmonary fibrosis (PF) from early-resolving COVID-PF, idiopathic pulmonary fibrosis (IPF), and non-diseased controls.
The findings, published in Frontiers in Immunology, could help doctors better personalize treatments for individual patients. The discovery will provide doctors with a useful tool to identify COVID-19 patients at risk for long-haul lung problems and help guide them to recovery.
UVA Health researchers have discovered a potential way to predict which patients with severe COVID-19 are likely to recover well and which are likely to suffer “long-haul” lung problems.
UVA’s new research also alleviates concerns that severe COVID-19 could trigger relentless, ongoing lung scarring akin to the chronic lung disease known as idiopathic pulmonary fibrosis, the researchers report. That type of continuing lung damage would mean that patients’ ability to breathe would continue to worsen over time.
“We are excited to find that people with long-haul COVID have an immune system that is different from people who have lung scarring that doesn’t stop,” said researcher Catherine A. Bonham, MD, a pulmonary and critical care expert who serves as scientific director of UVA Health’s Interstitial Lung Disease Program. “This offers hope that even patients with the worst COVID do not have progressive scarring of the lung that leads to death.”
Long-Haul COVID-19
Up to 30% of patients hospitalized with severe COVID-19 continue to suffer persistent symptoms months after recovering from the virus. Many of these patients develop lung scarring-some early on in their hospitalization, and others within six months of their initial illness, prior research has found. Bonham and her collaborators wanted to better understand why this scarring occurs, to determine if it is similar to progressive pulmonary fibrosis and to see if there is a way to identify patients at risk.
To do this, the researchers followed 16 UVA Health patients who had survived severe COVID-19. Fourteen had been hospitalized and placed on a ventilator. All continued to have trouble breathing and suffered fatigue and abnormal lung function at their first outpatient checkup.
After six months, the researchers found that the patients could be divided into two groups: One group’s lung health improved, prompting the researchers to label them “early resolvers,” while the other group, dubbed “late resolvers,” continued to suffer lung problems and pulmonary fibrosis.
Looking at blood samples taken before the patients’ recovery began to diverge, the UVA team found that the late resolvers had significantly fewer immune cells known as monocytes circulating in their blood. These white blood cells play a critical role in our ability to fend off disease, and the cells were abnormally depleted in patients who continued to suffer lung problems compared both to those who recovered and healthy control subjects.
Further, the decrease in monocytes correlated with the severity of the patients’ ongoing symptoms. That suggests that doctors may be able to use a simple blood test to identify patients likely to become long-haulers — and to improve their care.
“About half of the patients we examined still had lingering, bothersome symptoms and abnormal tests after six months,” Bonham said. “We were able to detect differences in their blood from the first visit, with fewer blood monocytes mapping to lower lung function.”
The researchers also wanted to determine if severe COVID-19 could cause progressive lung scarring as in idiopathic pulmonary fibrosis. They found that the two conditions had very different effects on immune cells, suggesting that even when the symptoms were similar, the underlying causes were very different. This held even in patients with the most persistent long-haul COVID-19 symptoms. “Idiopathic pulmonary fibrosis is progressive and kills patients within three to five years,” Bonham said. “It was a relief to see that all our COVID patients, even those with long-haul symptoms, were not similar.”
Because of the small number of participants in UVA’s study, and because they were mostly male (for easier comparison with IPF, a disease that strikes mostly men), the researchers say larger, multi-center studies are needed to bear out the findings. But they are hopeful that their discovery will provide doctors a useful tool to identify COVID-19 patients at risk for long-haul lung problems and help guide them to recovery.
“We are only beginning to understand the biology of how the immune system impacts pulmonary fibrosis,” Bonham said. “My team and I were humbled and grateful to work with the outstanding patients who made this study possible.”
Reference:
Grace C. Bingham, Chaofan Li, Yong Huang, Shwu-Fan Ma, Imre Noth, Jie Sun, High-dimensional comparison of monocytes and T cells in post-COVID and idiopathic pulmonary fibrosis, Frontiers in Immunology, https://doi.org/10.3389/fimmu.2023.1308594.