New Potential treatment found for patients suffering from Myasthenia Gravis: Study

For the thousands of people globally affected by the disease myasthenia gravis (MG), everyday activities become a struggle, and in severe cases, the disease can be life-threatening.
Until now, there has been no muscle-specific and effective treatment against this rare autoimmune disease that leads to severe weakening of the muscles and fatigue. But now, a team of researchers from Aarhus University reveals a breakthrough in the treatment of MG that could give hope to many patients worldwide.
“The patients simply became stronger because the new treatment improves the communication between motor nerves and muscle fibers,” says Thomas Holm Pedersen, an associate professor at the Department of Biomedicine at Aarhus University, CEO of NMD Pharma, and the lead author of the study that has just been published in the journal Science Translational Medicine.
Focusing on the link between nerve cells and muscles
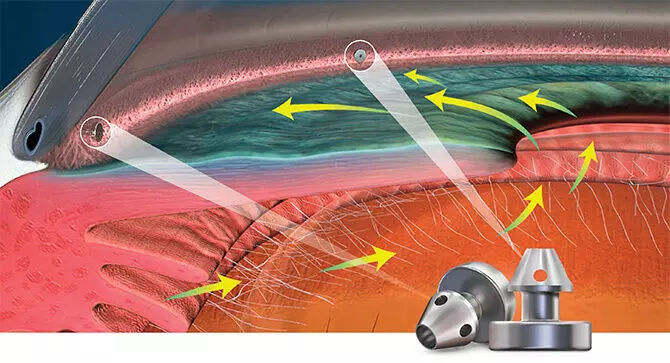
MG is a disease where the immune system attacks the connection between nerves and muscle cells. It can affect breathing and be life-threatening, and it was precisely these symptoms that the researchers aimed to combat by strengthening the function of the contact point between nerves and muscle cells.
During his PhD project at Aarhus University, Thomas Holm Pedersen discovered that the so-called CIC-1 chloride channels at the neuromuscular junction are crucial for muscle activation.
“This led to the idea of using the CI channels as a new treatment point for diseases where the neuromuscular connection is compromised, including myasthenia gravis,” he explains.
And it proved to be a good idea. The researchers demonstrated that they could effectively strengthen the muscles’ ability to respond to nerve impulses by targeting a treatment at the specific channel. This, in theory, could increase muscle strength and reduce fatigue in patients.
“As there were no medications targeting the Cl channel, we first had to find the right molecule that we could test in patients, which requires considerable work and various tests before the regulatory authorities allow testing in humans. We tested it on patients who had to take a tablet daily for their muscle weakness and fatigue, and we could see that the treatment concept worked. The patients became stronger.
Treatment without side effects?
This represents a significant advance in the treatment of MG. Not only because it was successful in increasing muscle strength among patients, but also because the treatment, unlike existing methods, may well prove to be free from side effects.
“We won’t know for sure for a few years, after we’ve conducted more studies, but it looks really promising right now,” says Thomas Holm Pedersen.
The breakthrough could result in a significant improvement in the quality of life for patients struggling with MG, but it is also a big leap forward in the understanding and treatment of other neuromuscular diseases.
The research team is currently planning more follow-up clinical trials, including another study on MG and one on the hereditary disease spinal muscular atrophy, which leads to muscle wasting.
According to Thomas Holm Pedersen, we may be on the verge of a paradigm shift in the treatment of MG and other serious neuromuscular diseases.
“This study summarizes years of work here at Aarhus University and NMD Pharma. We have proven that the method works in patients, and now we continue with the clinical trials to bring the drug to the patients and to explore its broader application,” he says.
Reference:
Martin Skov et al. ,The ClC-1 chloride channel inhibitor NMD670 improves skeletal muscle function in rat models and patients with myasthenia gravis.Sci. Transl. Med.16,eadk9109(2024).DOI:10.1126/scitranslmed.adk9109.
Powered by WPeMatico