Daily aspirin can significantly reduce liver fat content in metabolic dysfunction-associated steatotic liver disease: Study
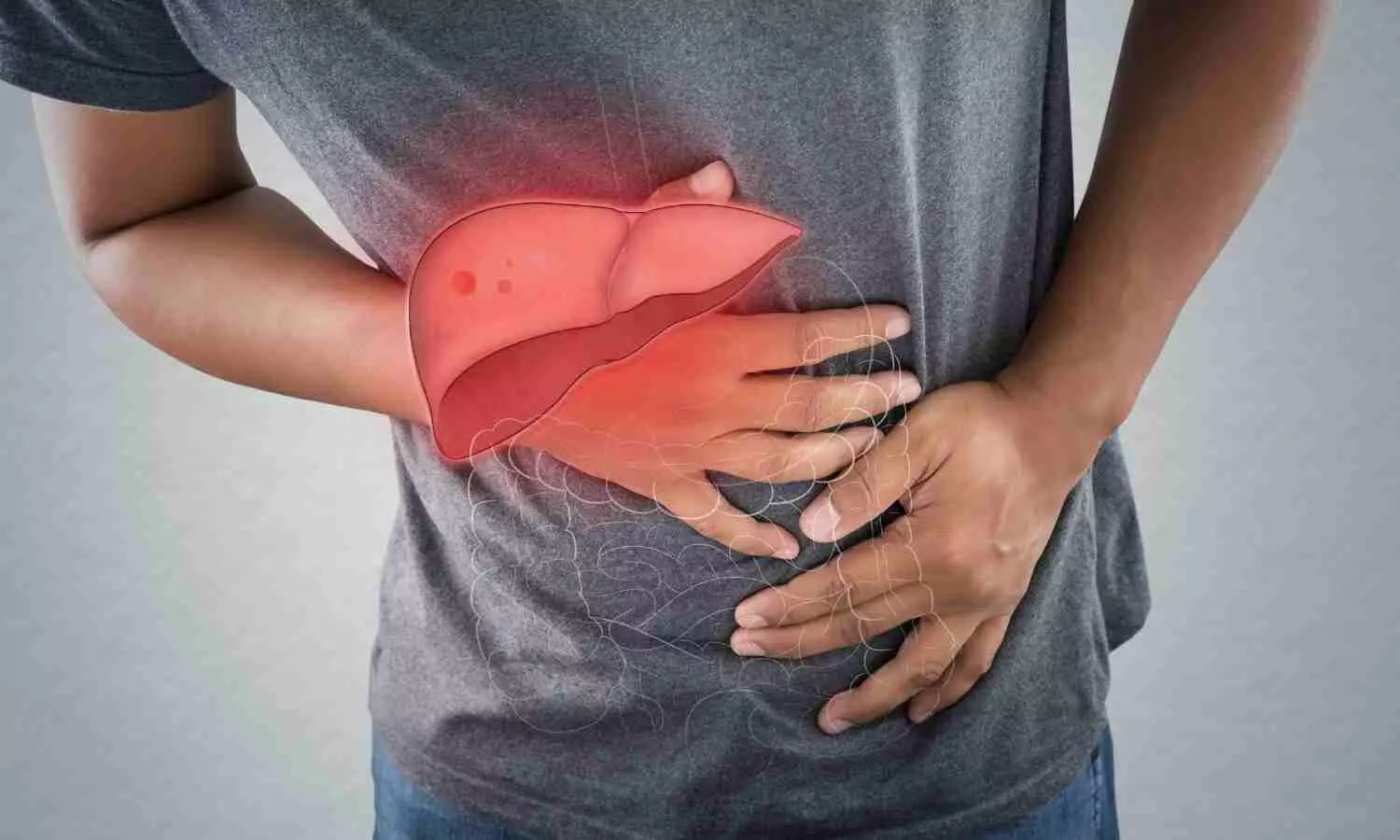
USA: A recent clinical trial revealed that six months of daily low-dose aspirin significantly reduced hepatic fat quantity compared with placebo in patients with metabolic dysfunction-associated steatotic liver disease (MASLD).
The most common chronic liver disease is metabolic dysfunction-associated steatotic liver disease characterized by an increased buildup of fat in the liver due to factors such as obesity and type 2 diabetes.
Such elevated fat poses serious health risks, but the clinical trial published in JAMA and conducted by investigators from Massachusetts General Hospital, a founding member of the Mass General Brigham healthcare system, reveals that daily aspirin can significantly reduce liver fat content.
“Since MASLD is estimated to affect up to a third of U.S. adults, aspirin represents an attractive potential low-cost option to prevent progression to cirrhosis or liver cancer, the most feared complications of MASLD,” said senior author Andrew T. Chan, MD, MPH, a gastroenterologist and chief of the Clinical and Translational Epidemiology Unit at Massachusetts General Hospital.
Chan and his colleagues tested aspirin’s potential because the drug reduces inflammation and affects fat metabolism.
In their phase 2 trial, 80 adults with MASLD were randomized to receive daily low-dose aspirin (81 mg) or placebo for six months.
At the end of the trial, the average change in liver fat content was -6.6% with aspirin versus +3.6% with placebo, indicating that low-dose aspirin reduced the average liver fat content by 10.2% compared with placebo. Low-dose aspirin was found to be safe and well-tolerated.
Aspirin also improved various markers of liver health. “Multiple non-invasive blood and imaging-based tests for liver fat, inflammation, and fibrosis all showed a similar direction of benefit that favored aspirin treatment,” said lead author and Principal Investigator Tracey G. Simon, MD, MPH, a hepatologist in the Division of Gastroenterology at Massachusetts General Hospital. “Together, these data support the potential for aspirin to provide benefits for patients with MASLD.”
References: Tracey G. Simon, MD, MPH1,2,3; Robert M. Wilechansky, MD1,2,4; Stefania Stoyanova, BA4; et al JAMA. 2024;331(11):920-929. doi:10.1001/jama.2024.1215
Powered by WPeMatico