Higher long-term variability of serum uric acid associated with diabetic retinopathy risk: Study
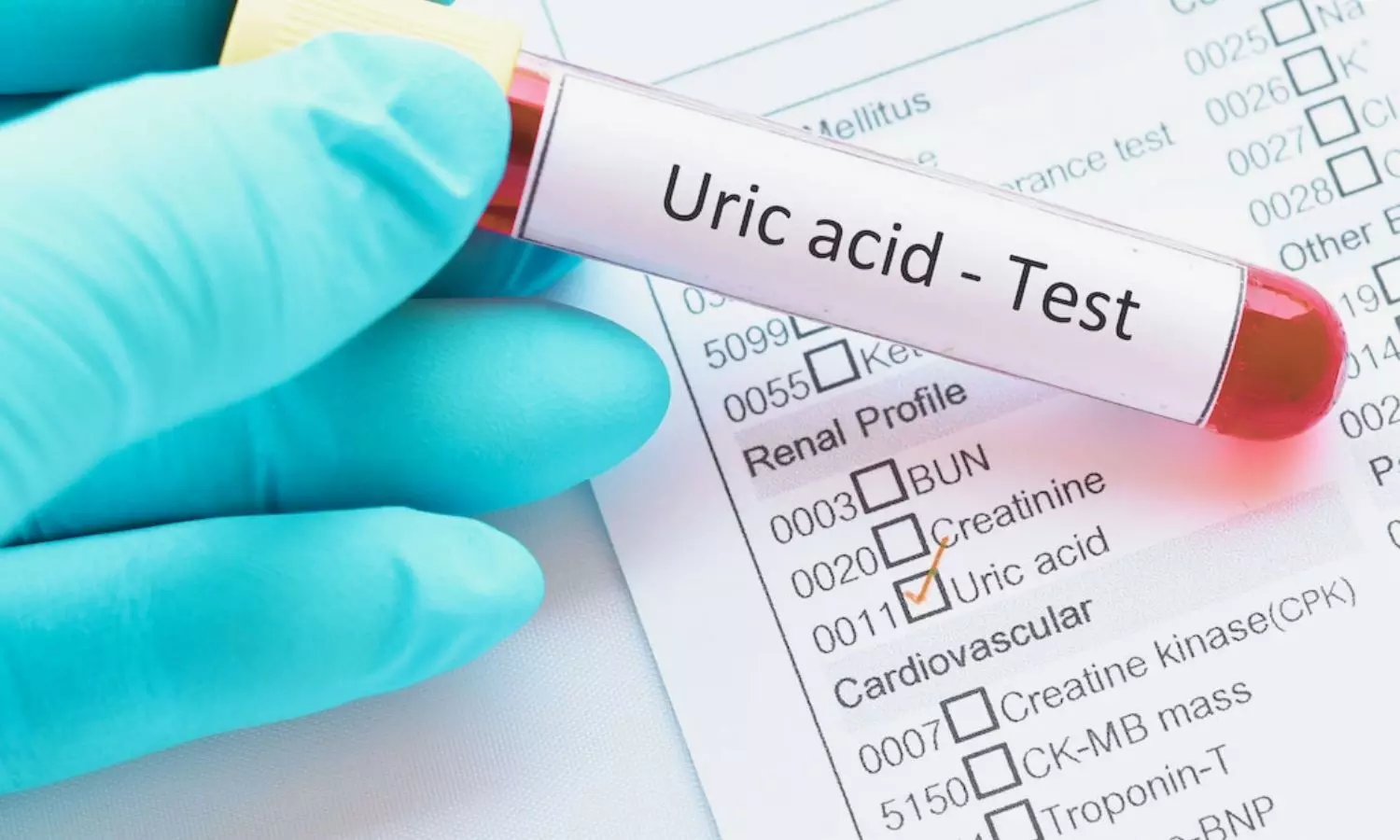
A new study published in the journal of Diabetes Research and Clinical Practice found that patients with type 1 and type 2 diabetes mellitus had a greater chance of developing diabetic retinopathy (DR) if their serum uric acid levels were variable.
With a projected global incidence of 12.2% in 2045, diabetes mellitus (DM), a metabolic condition marked by persistent hyperglycemia brought on by absolute or relative insulin insufficiency, has emerged as one of the most prevalent chronic illnesses. Diabetes-related hyperglycemia and other metabolic irregularities can have a significant impact on the body’s organs, resulting in retinopathy, nephropathy, and neuropathy, among other problems.
One significant ocular consequence of diabetes is DR, which affects 22.27 percent of people with diabetes. Additionally, 6.17 percent of people with diabetes have vision-threatening DR (VTDR), making DR the most common cause of visual impairment in people of working age.
Purine metabolism produces uric acid, and high blood uric acid levels are a frequent metabolic change seen in diabetic patients. Several clinical investigations have linked higher serum uric acid levels to diabetic retinopathy. Thus, this study assessed the relationship between the onset and/or severity of diabetic retinopathy (DR) in patients with Type 1 and Type 2 diabetes mellitus (DM) and the variability of serum uric acid (SUA).
At Shanghai General Hospital, 730 DM patients lacking proliferative diabetic retinopathy at baseline participated in a prospective trial. Every subject had several DR evaluations using fundus photography and SUA measures throughout the course of at least a year of follow-up. To evaluate SUA fluctuations, average real variability (ARV) was computed for every patient, taking into consideration different follow-up frequencies and visit counts.
With a Log-rank p-value of 0.0055, the Kaplan-Meier survival analysis revealed that the group with higher SUA ARV scores had a greater chance of developing and progressing DR.
The hazard ratios for DR deterioration in patients in the third and fourth quantiles of ARV are 2.2 (p = 0.008, 95 % CI: 1.2206∼3.8201) and 2.74 (p = 0.017, 95 % CI: 1.1339∼3.7255), respectively, as compared to patients in the first quantile, according to Cox regression with Backward Stepwise Selection of covariates.
Overall, in DM patients, high long-term variability is strongly linked to the onset and exacerbation of DR, indicating the significance of the advantages of ongoing serum uric acid management.
Source:
Zhu, Q., Wang, H., Qu, Y., Jiang, Y., Liu, X., Liu, X., Xiao, Y., Lv, K., Xing, X., Niu, T., & Liu, K. (2025). Association between long-term serum uric acid variability and diabetic retinopathy: A prospective study in patients with Type 1 and Type 2 diabetes. Diabetes Research and Clinical Practice, 226(112306), 112306. https://doi.org/10.1016/j.diabres.2025.112306
Powered by WPeMatico