CDSCO Flags MSD Pharma’s Cancer Drug Trial Over Indian Representation, Control Arm

New Delhi: The Subject Expert Committee (SEC) on Oncology under the Central Drugs Standard Control Organization (CDSCO) has raised critical concerns over the Phase III clinical trial proposal of Sacituzumab Tirumotecan submitted by MSD Pharmaceuticals Pvt. Ltd., directing the company to provide detailed justifications regarding its study design and patient representation in India.
MSD Pharmaceuticals Pvt. Ltd., the Indian subsidiary of global biopharmaceutical company Merck & Co., presented its Phase III clinical trial Protocol No. MK2870-032, Version 00, dated February 18, 2025, for evaluation.
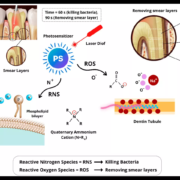
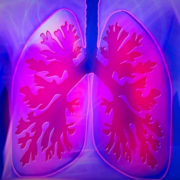
Sacituzumab Tirumotecan is an investigational antibody-drug conjugate (ADC) being developed for the treatment of various cancers, including triple-negative breast cancer and metastatic urothelial carcinoma. The drug combines a humanized monoclonal antibody targeting the Trop-2 receptor with a cytotoxic topoisomerase I inhibitor payload, enabling selective delivery of chemotherapy directly to tumor cells while minimizing systemic toxicity.
During the SEC review, the committee identified two significant issues. Firstly, the proposed control arm in the study was not aligned with the current standard of care, prompting the SEC to ask the company for a clear scientific rationale behind its selection. Secondly, the committee noted that the proposed inclusion of only 60 Indian patients – representing less than 3% of the global trial population of 2,400—was inadequate to generate statistically meaningful outcomes for the Indian population.
The SEC emphasized that such limited representation could compromise the reliability and applicability of trial results in India, potentially affecting regulatory evaluation and future patient access. In light of this, the committee requested MSD Pharmaceuticals to substantially increase the Indian sample size to ensure appropriate representation and robust statistical validity.
After detailed deliberation, the SEC directed the company to submit comprehensive justifications regarding the control arm choice and provide a revised study plan with an expanded Indian cohort. The committee clarified that the trial cannot proceed for further consideration until these issues are adequately addressed, reinforcing the importance of robust trial design and sufficient patient representation for global oncology studies conducted in India.
Powered by WPeMatico