A study published in the journal Scientific Reports indicates that physical exercise combined with omega-3 supplementation considerably improves the immune response and reduces the severity of chronic apical periodontitis.
Inflammation at the apex of the tooth – the tip of the root – and in the surrounding area is primarily caused by caries. If left untreated, the bacteria can reach the root canal and pass through it to the apex, causing apical periodontitis. This condition leads to bone loss in the area.
The study is the first to demonstrate that a combination of moderate physical exercise and omega-3 supplementation significantly improves the inflammatory condition caused by apical periodontitis. This combination limited bacterial progression, reduced bone tissue loss, regulated the release of pro-inflammatory cytokines, and stimulated the activity of fibroblasts, the cells that create and maintain tissue.
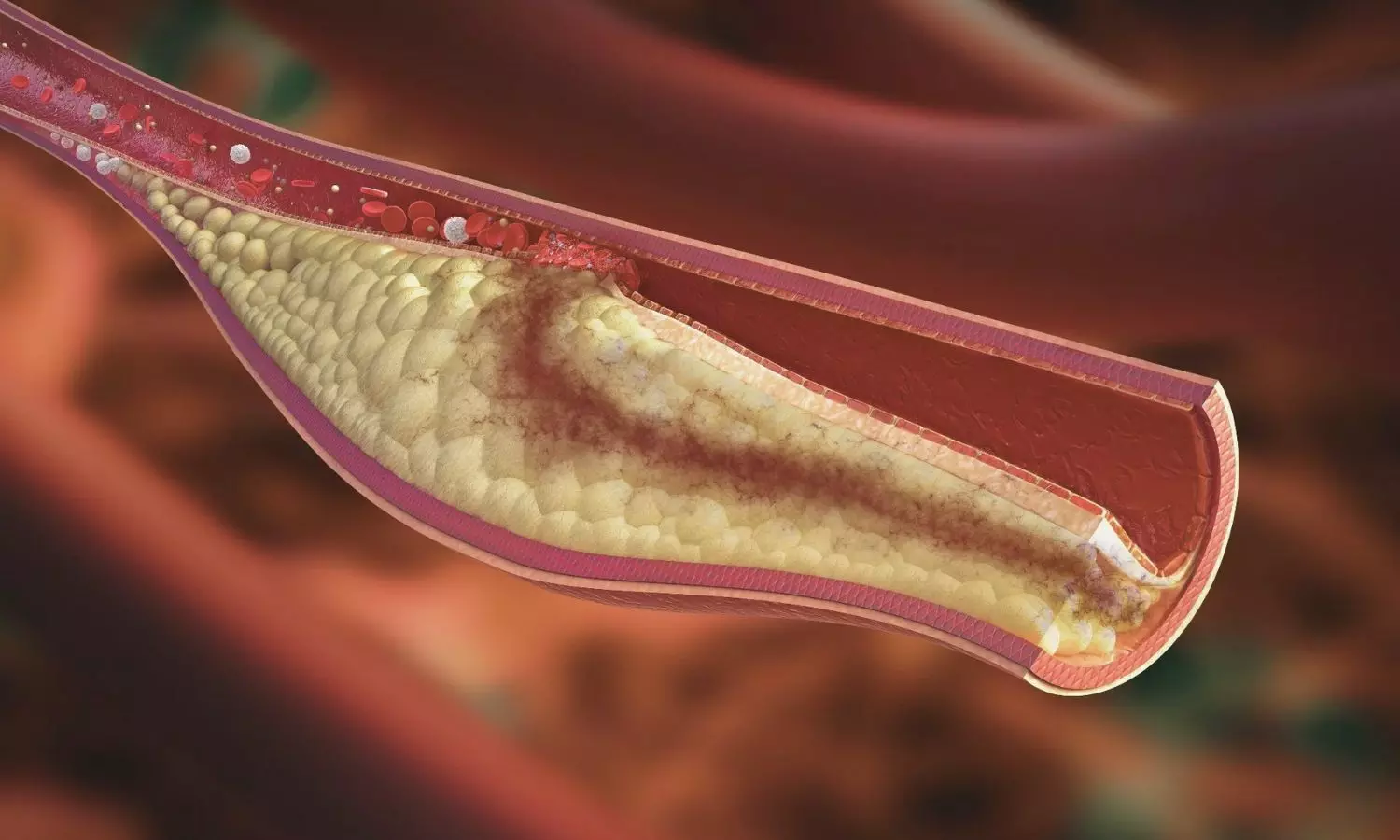
If left untreated, the infection can lead to tooth loss. In addition, there is a two-way relationship between apical periodontitis and systemic changes in patients. Diabetes, metabolic syndrome, arteriosclerosis, and kidney disease, among others, can exacerbate apical periodontitis. At the same time, infection in the apex can exacerbate these diseases.
“It’s a condition that patients may not even know they have because of its chronic nature, but which can evolve and lead to bone destruction and tooth mobility. In addition, in specific situations, such as a drop in immunity, it can become acute, so the patient starts to feel pain, pus forms at the site, the face can become swollen,” explains Rogério de Castilho, a professor at the Araçatuba School of Dentistry at São Paulo State University (FOA-UNESP) in Brazil. Castilho supervised the study and is supported by FAPESP.
“In rats, physical exercise alone brought about a systemic improvement, regulating the local immune response. In addition, when combined with supplementation, it further reduced the destructive condition caused by endodontic pathology,” explains Ana Paula Fernandes Ribeiro, the first author of the study, carried out during her doctorate at FOA-UNESP.
Less inflammation
The researchers induced apical periodontitis in 30 rats and divided them into three groups. The first group received no intervention. The second and third groups underwent a 30-day swimming regimen.
The third group also received dietary supplementation of omega-3, a polyunsaturated fatty acid known for its therapeutic effects on chronic inflammatory diseases.
The group that only swam had better outcomes than the untreated control group. However, omega-3 supplementation combined with physical exercise regulated the immune response and infection control even better.
Immunohistochemical analyses, which assess how the immune system responds to infection, revealed varying levels of the cytokines interleukin 17 (IL-17) and tumor necrosis factor alpha (TNF-α), indicating the intensity of the inflammatory response.
While the rats that received no treatment had moderate levels of these cytokines, those that exercised had lower levels, and those that took supplementation had the lowest levels.
In addition to having lower levels of these cytokines, the group that exercised had fewer osteoclasts. These are cells that resorb bone tissue, indicating bone loss. The results were even better for the group that consumed omega-3, showing statistically significant differences compared to the animals that received no treatment.
Micro CT scans of the jaws showed that the animals that swam experienced less loss of volume of alveolar bone, which covers the teeth, than those in the control group. The loss was even less in the supplemented group.
For the authors, the study provides new evidence of the benefits of physical activity and omega-3 for the immune system, now with even more obvious repercussions for oral health.
“To know if the same would be true for humans, we’d need a clinical study with a significant number of patients. However, in addition to the many proven benefits of physical exercise and omega-3 consumption, this is yet another important piece of evidence,” Jacinto says.
Reference:
Ribeiro, A.P.F., de Lima Rodrigues, M., Loureiro, C. et al. Physical exercise alone or combined with omega-3 modulates apical periodontitis induced in rats. Sci Rep 15, 8760 (2025). https://doi.org/10.1038/s41598-025-90029-9