Obstructive Sleep Apnea Doubles Risk of Severe Glaucoma Progression, Study Finds
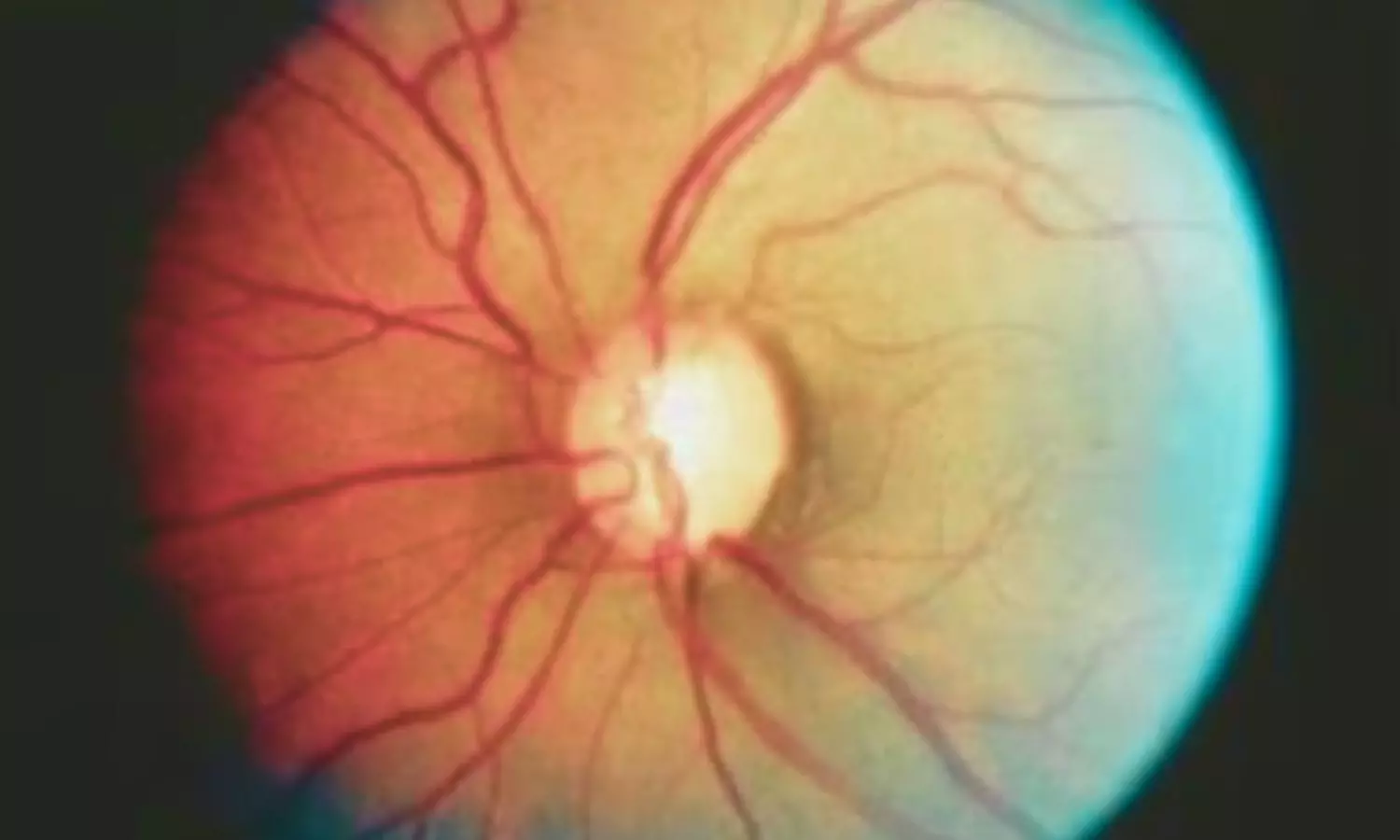
USA: Patients diagnosed with obstructive sleep apnea (OSA) may be at a significantly higher risk of rapid glaucoma progression, according to a new study that evaluated the long-term outcomes of primary open-angle glaucoma (POAG) in those with and without OSA. The research, published in Ophthalmology Glaucoma, emphasizes the need for early and potentially more aggressive intervention to help mitigate vision loss in this high-risk group.
Led by Dr. Pranav Vasu from the Department of Medicine at Creighton University School of Medicine, Phoenix, Arizona, the study analyzed data from the TriNetX US Collaborative Network using electronic health records spanning from January 2004 to October 2024. The retrospective cohort included 5,277 patients with OSA and 5,277 without, all of whom had mild to moderate POAG at baseline.
The investigators examined the risk of progressing to severe POAG over 3-, 5-, and 10-year follow-up periods.
The study led to the following findings:
- Patients with obstructive sleep apnea (OSA) had significantly higher odds of progressing to severe glaucoma after adjusting for baseline characteristics, comorbidities, and medication use.
- The risk of progression to severe glaucoma was nearly 2.8 times higher at 3 years for patients with OSA compared to those without.
- At 5 years, the odds of disease progression were 2.3 times higher for the OSA group.
- After 10 years, the risk remained elevated, with just over 2.1 times higher odds of severe glaucoma among those with OSA.
- There was no significant difference in the rates of minimally invasive glaucoma surgeries (MIGS) or trabeculectomy procedures between patients with and without OSA.
- Laser treatments and tube shunt surgeries were significantly more common in patients with OSA at all follow-up time points.
“These findings suggest that while OSA patients face a markedly greater risk of glaucoma progression, surgical interventions such as MIGS and trabeculectomy are not necessarily used more frequently,” the authors noted. “Instead, there is greater reliance on laser therapies and tube shunt procedures, which may reflect the need to address more advanced or rapidly progressing disease in this group.”
The study highlights the importance of recognizing OSA as a potential accelerator of POAG and suggests that standard management strategies may not be sufficient for this subset of patients. Clinicians are encouraged to consider early screening and timely interventions tailored to individuals with coexisting OSA and glaucoma to help prevent irreversible vision loss.
In light of these findings, the authors advocate for greater clinical vigilance and suggest revisiting current treatment algorithms for POAG patients with OSA. Proactive management, they argue, could help alter the course of disease and preserve visual outcomes over time.
Reference:
Vasu, P., Wagner, I. V., Lentz, P. C., Gumaste, P., Abubaker, Y., Ang, B. C., Ahuja, A. S., Dorairaj, E., Qozat, I., Miller, D. D., & Dorairaj, S. (2025). Obstructive Sleep Apnea as a Potentiator of Primary Open Angle Glaucoma and Necessity for Interventional Therapy. Ophthalmology Glaucoma. https://doi.org/10.1016/j.ogla.2025.05.005
Powered by WPeMatico