Pick up the pace of your daily walk to boost longevity, experts say
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

A recent analysis of U.S. population-based cohorts has revealed that early-onset chronic obstructive pulmonary disease (COPD) — diagnosed in individuals aged 18 to 49 — affects at least 4.5% of this age group and is tied to significantly higher long-term health risks. These include increased hospitalization rates, elevated risk of chronic lower respiratory disease mortality, a greater likelihood of developing heart failure, and higher all-cause mortality before age 75 (Lange et al., 2024).
The study, published in NEJM Evidence, highlights a growing concern: COPD is not just a disease of older adults. While traditionally associated with long-term smoking in older populations, early-onset COPD may result from multiple exposures — including secondhand smoke, environmental pollutants, vaping, and early-life respiratory infections — and often goes underdiagnosed in younger adults. Researchers suggest that defining and recognizing “early COPD” as a distinct clinical category could help identify at-risk individuals sooner and offer a critical window for intervention. Despite their younger age, patients with early COPD experience significant declines in lung function and quality of life and are more likely to develop comorbid conditions like cardiovascular disease. vThe findings point toward a need for earlier screening strategies, especially in young adults with chronic respiratory symptoms or known risk factors. Proactive management — including smoking cessation, pulmonary rehab, and timely pharmacotherapy — could potentially alter the trajectory of the disease.
Keywords: early-onset COPD, chronic respiratory disease, COPD in young adults, lung health, premature mortality, all-cause mortality, heart failure risk, respiratory hospitalization, U.S. cohorts, COPD risk factors, Lange, P., Barr, R. G., Hansel, N. N
Powered by WPeMatico
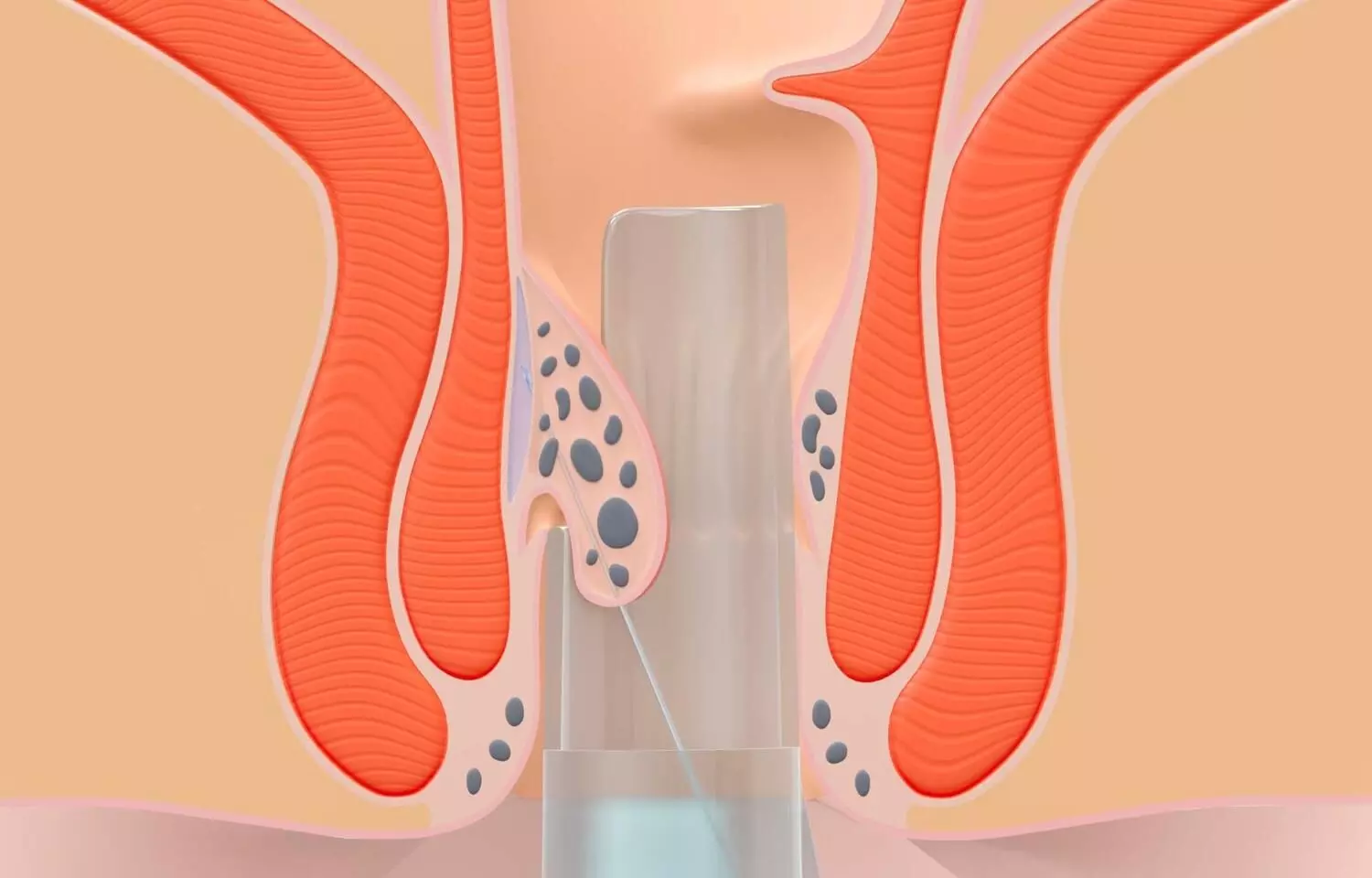
Researchers have found in a new study that minimally invasive tissue-selecting therapy (TST) is effective in managing severe hemorrhoids, significantly enhances anorectal motility, and demonstrates a low rate of postoperative complications, indicating a high level of safety.
Severe hemorrhoids have a serious impact on patients’ quality of life. At present, the main method for treating severe hemorrhoids is surgery, but surgical treatment causes greater trauma to patients and has a high degree of complications. There is an urgent need to find new surgical methods to solve these problems. To assess the ability of tissue-selective therapy stapler (TST) minimally invasive surgery to treat severe hemorrhoids by studying the clinical efficacy, postoperative complications, and anal dynamics of selective supramedullary hemorrhoid stomy. In the hospital, between March 2015 and February 2018, 141 patients with severe hemorrhoids were included into three groups according to the block randomization method: the TST group, the pieces per hour the PPH group, and the eastern rubber band ligation and coincident of dislocation for prolapse and hemorrhoid (EPH)group. There were 47 patients in each group. The clinical efficacy of the three groups of patients, changes in hospital stay time, operation time, intraoperative blood loss, postoperative complications, and anal dynamic indicators (rectal resting pressure, anal resting pressure, anorectal pressure difference, rectal tolerance, rectal perception threshold and length of the anal high-pressure zone) were observed and compared. Results: The total effective rate in the TST group was 93.62%, which was higher than the 74.47% and 72.34% in the PPH and EPH groups, respectively, after treatment. Hospitalization time, operation time, and intraoperative blood loss were lower in the TST group than in the EPH and PPH groups. Three months after surgery, the rectal resting pressure, rectal tolerance, and rectal sensing thresholds of patients in the TST group were lower than those in the PPH and EPH groups, and the anal canal resting pressure, the anorectal pressure difference and the length of the anal high-pressure zone were greater than those in the PPH and EPH groups. After surgery, the complication rate in the TST group was 10.64%, which was lower than the 27.66% and 31.91% reported in the PPH and EPH groups, respectively. Minimally invasive TST is effective in treating severe hemorrhoids, can significantly improve anorectal motility, has a low incidence of postoperative complications and is highly safe.
Reference:
Huang, R., Fan, M., Lin, H. et al. Tissue selecting therapy stapler minimally invasive surgery to treat severe hemorrhoids. BMC Surg 25, 293 (2025). https://doi.org/10.1186/s12893-025-02918-5
Keywords:
1500X 600 Minimally, Invasive, tissue-selecting, therapy, Effective, Safe, Severe, Hemorrhoids, reveals, research, Huang, R., Fan, M., Lin, H, Selective suprahemorrhoidal, mucosa anastomosis, Severe hemorrhoids, Clinical efficacy, Complications, Anal dynamics
Powered by WPeMatico

A new study published in the Journal of American Medical Association showed that when compared to standard therapy, remote, scalable cognitive behavioral therapy skills training programs for chronic pain (CBT-CP) therapies (either through telehealth or self-completed online courses) produced moderate reductions in pain and associated functional/quality-of-life outcomes in people with high-impact chronic pain.
Although they are not generally available, cognitive behavioral therapy (CBT) skills training programs are advised as the initial nonpharmacologic treatment for chronic pain. Thus, this study was set to evaluate the efficacy of telehealth and self-completed online remote, scalable CBT-CP therapies with standard care for those with high-impact chronic pain.
From January 2021 to February 2023, 2331 eligible individuals with high-impact chronic musculoskeletal pain from four geographically disparate US health care systems participated in this comparative efficacy, 3-group, phase 3 randomized clinical research. The period of follow-up ended in April 2024.
The participants were randomly assigned 1:1:1 to one of two remote, 8-session CBT-based skills training treatments: normal care with a resource guide (n = 777) or a health coach-led program via videoconference or phone (health coach; n = 778) or an online self-completed program (painTRAINER; n = 776).
Achieving or surpassing the minimum clinically meaningful difference (MCID) in pain intensity score (≥30% drop; score range, 0-10) on the 11-item Brief Pain Inventory–Short Form between baseline and 3 months was the main goal. Pain severity, pain-related interference, PROMIS (Patient-Reported Outcomes Measurement Information System) social role and physical functioning, and the patient’s overall perception of change were secondary outcomes at 3, 6, and 12 months.
A total of 2,210 (94.8%) of the 2,331 eligible randomized participants finished the trial. The adjusted proportion of individuals who experienced a 30% or more reduction in their pain severity score at 3 months was 26.6 (95% CI, 23.4-30.2) in the painTRAINER group, 20.8 (95% CI, 18.0-24.0) in the usual care group, and 32.0 (95% CI, 29.3-35.0) in the health coach group.
The relative risk [RR] for both intervention groups was 1.54 [95% CI, 1.30-1.82] when compared to the control group. The RR for painTRAINER versus usual care was 1.28 [95% CI, 1.06-1.55]; and the RR for the health coach program was 1.20 [95% CI, 1.03-1.40] when compared to the online self-completed painTRAINER program.
At 6 and 12 months following randomization, both intervention groups showed statistically significant improvements in pain severity outcomes as well as various secondary pain and functional outcomes as compared to conventional treatment. Overall, the results indicate that centralizing the delivery of CBT-CP-based programs using online interventions and telephone/videoconferencing is successful.
Reference:
DeBar, L. L., Mayhew, M., Wellman, R. D., Balderson, B. H., Dickerson, J. F., Elder, C. R., Justice, M., Keefe, F. J., McMullen, C. K., Owen-Smith, A. A., Rini, C., Von Korff, M., Waring, S., Yarava, A., Shen, Z., Thompson, R. E., Clark, A. E., Casper, T. C., & Cook, A. J. (2025). Telehealth and online cognitive behavioral therapy-based treatments for high-impact chronic pain: A randomized clinical trial: A randomized clinical trial. JAMA: The Journal of the American Medical Association. https://doi.org/10.1001/jama.2025.11178
Powered by WPeMatico
