Timely diagnosis and proper management of peripheral artery disease (PAD), including coordinated care from a multispecialty team, are essential to help prevent amputation and other cardiovascular complications and to allow patients with PAD to live longer lives with better physical function and improved quality of life, according to a new joint guideline published today in the American Heart Association’s flagship, peer-reviewed journal Circulation and simultaneously in the Journal of the American College of Cardiology.
The “2024 AHA/ACC Guideline on the Management of Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines” provides the latest, evidence-based recommendations to guide clinicians in the diagnosis and treatment of lower extremity PAD across its four clinical presentation subsets: asymptomatic disease, chronic symptomatic PAD, and the more severe subsets of chronic limb-threatening ischemia (CLTI) and acute limb ischemia (ALI).
In addition to being led by the American Heart Association and the American College of Cardiology Joint Committee on Clinical Practice Guidelines, the guideline was developed with and endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Podiatric Medical Association, the Association of Black Cardiologists, the Society for Cardiovascular Angiography and Interventions, the Society for Vascular Medicine, the Society for Vascular Nursing, the Society for Vascular Surgery, the Society of Interventional Radiology and the Vascular & Endovascular Surgery Society.
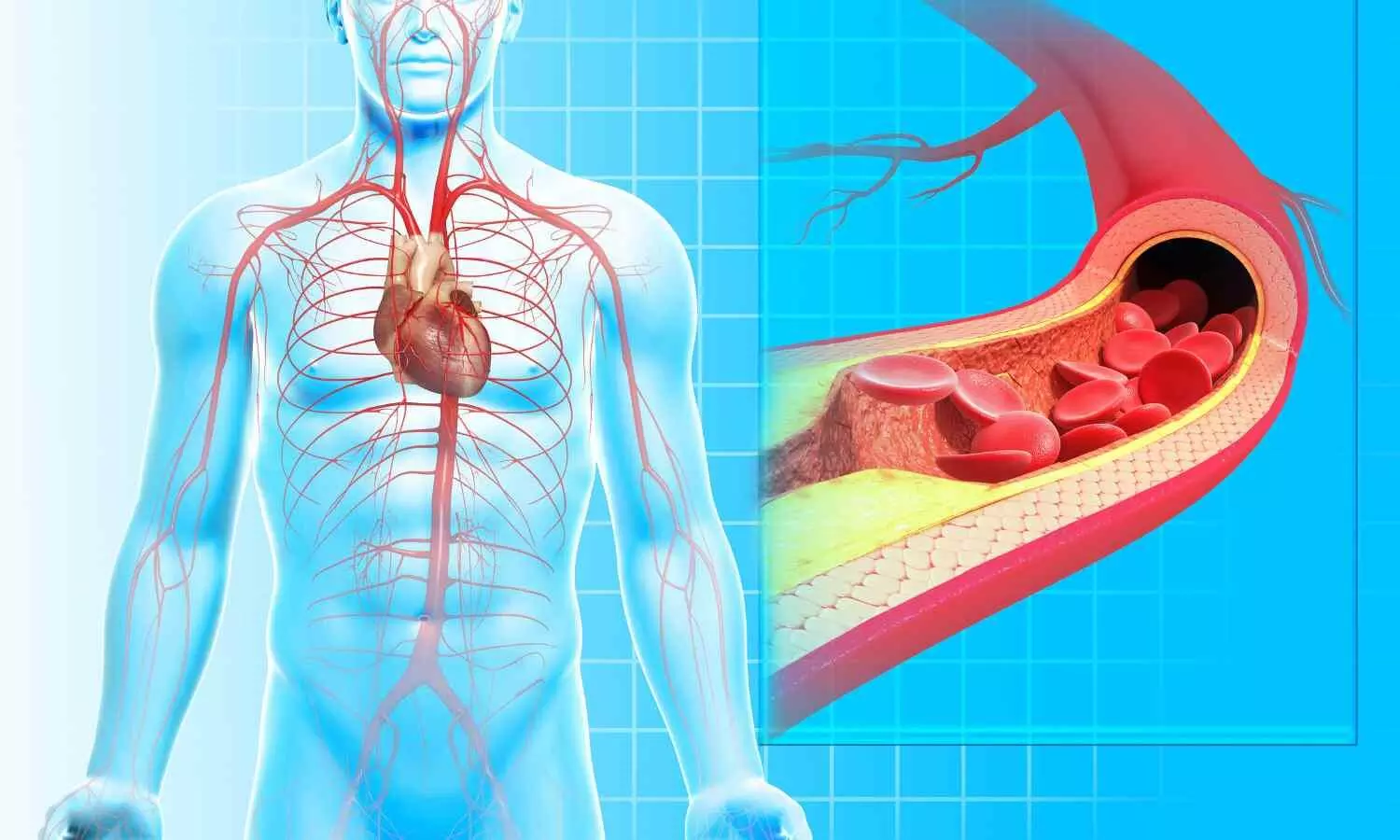
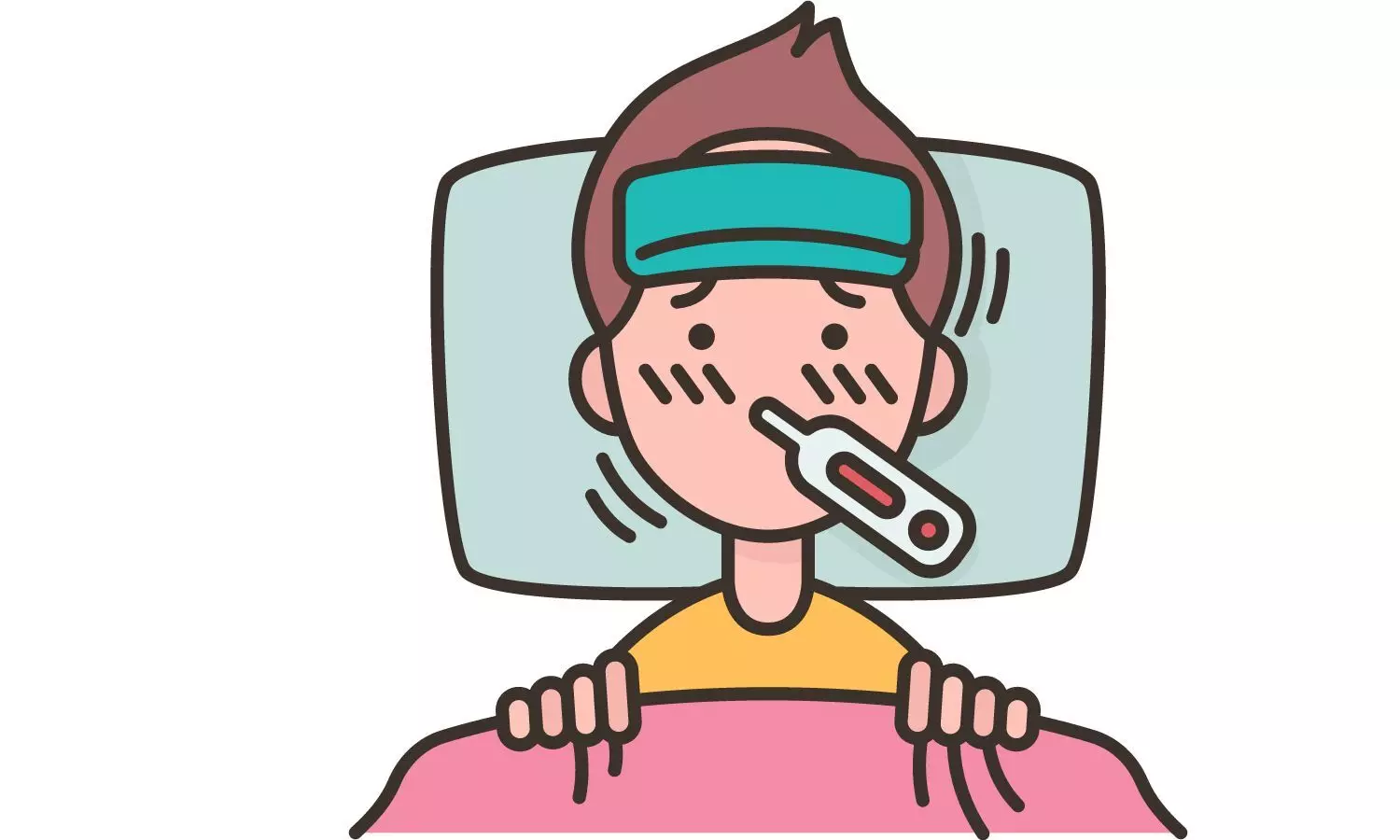
PAD is a serious, progressive cardiovascular disease primarily caused by a buildup of fatty plaque in the blood vessels, or atherosclerosis. This plaque narrows the blood vessels and reduces blood flow to the legs and feet, which may significantly impair physical function, walking performance and quality of life. Approximately 10 million to 12 million adults ages 40 and older in the U.S. have PAD, which increases the risk of amputation, heart attack, stroke and death. Among those ages 65 and older, nearly 50% who underwent limb amputation died within one year after surgery, according to the 2024 Heart Disease and Stroke Statistics: A Report of U.S. and Global Data From the American Heart Association. Risk factors for PAD include smoking; having Type 1 or Type 2 diabetes, high blood pressure, high cholesterol, chronic kidney disease, atherosclerosis in other parts of the body (such as coronary artery disease); and being age 75 years or older.
Effective medical therapies and coordinated care
Once PAD is diagnosed, implementing a plan of care, including guideline-directed medical therapies and management of PAD-related risk amplifiers, is crucial to reduce the risk of progression to more symptomatic and limb-threatening clinical presentations of PAD and to reduce the risk of amputation, heart attack, stroke and death. Although there are highly effective medical, endovascular and surgical therapies for PAD, historically, many people with PAD have been undertreated or do not receive guideline-directed medical therapies at the same rate as peers with other cardiovascular diseases, such as coronary artery disease.
“Because of the complexities of PAD, to improve outcomes and reduce the risk of limb loss for these patients, a multispecialty care team approach that is focused on comprehensively addressing risk factor management, foot care and revascularization is needed to promote collaboration, avoid duplication of care and optimize patient outcomes,” said Chair of the guideline writing committee Heather Gornik, M.D., FAHA, co-director of the Vascular Center at the University Hospitals Harrington Heart & Vascular Institute and a professor of medicine at Case Western Reserve University School of Medicine, both in Cleveland, Ohio.
Effective medical therapies for patients with PAD, including medications to prevent blood clotting, manage blood sugar and reduce high blood pressure and high cholesterol, should be prescribed to prevent major adverse cardiovascular events and reduce the risk of amputation. All patients with PAD should be treated with high-intensity statin therapy. For people with PAD who are not at an increased risk of bleeding, new evidence supports the use of low-dose rivaroxaban (2.5 mg twice daily) combined with low-dose aspirin (81 mg daily).
For patients with PAD and Type 1 or Type 2 diabetes, clinicians should coordinate care to address diet, exercise, weight management, medications to control blood sugar, management of other cardiovascular risk factors and routinely check the feet of their patients for foot ulcer prevention. Foot care is important for patients across the four clinical presentation subsets of PAD. Comprehensive treatment includes patient education, preventive foot care, more intensive wound care and pressure off-loading to minimize amputation in patients with more severe forms of PAD.
Health care professionals should also encourage patients to quit smoking or using other forms of tobacco to reduce the risk of developing PAD, to slow the progression of established PAD and to reduce the risk of limb-related conditions or death. Pharmacological and behavioral-based strategies often increase the smoking cessation rate in people with PAD, however, these strategies are underused.
A core component of care for patients with symptomatic PAD is structured exercise therapy programs, including both community- and home-based programs, as well as supervised exercise therapy delivered in a clinic or hospital setting. Multiple studies have shown that these programs improve functional status, walking performance and quality of life compared to usual care.
“Supervised exercise therapy, the gold standard exercise therapy for patients with PAD, is woefully underutilized despite its known health benefits and the fact that it is covered by Medicare and most health insurance plans,” said Gornik. “Rates of referral for supervised exercise therapy among PAD patients are incredibly low. It has been estimated that less than 5% of patients with PAD in the U.S. are prescribed to participate in a supervised exercise program.”
If left untreated, PAD may progress to severe forms known as chronic limb-threatening ischemia (CLTI) and acute limb ischemia (ALI). Both are the result of severe blockage in the arteries of the legs that significantly reduces blood flow, causes pain in the legs at rest or with minimal activity, impairs physical function and significantly increases the risk of amputation and death. For these patients, timely diagnosis and treatments, including revascularization procedures to reconstruct diseased arteries, are essential to prevent tissue loss and preserve the limb. Endovascular (a catheter procedure), surgical or hybrid revascularization techniques may be performed to improve blood flow to the limb, with the goals of healing wounds, relieving PAD-associated pain, maintaining walking ability and preventing amputation.
Disparities in risk factors for PAD and health outcomes
The disparities in PAD care and outcomes are significant among people from under-resourced communities in the U.S. Black adults have a nearly 30% lifetime risk of developing PAD compared to 19% for white adults. Black adults with PAD in the U.S. are often identified at a more advanced stage and have a four-fold higher rate of major limb amputation, 30% higher heart disease mortality rate and 45% higher rate of stroke compared to white adults.
Social determinants of health, and other factors such as race and ethnicity, disparities in housing, health care access, education and socioeconomic status, may also affect the prevalence of PAD and patient outcomes.
“Racial and ethnic disparities in the detection, management and health outcomes of PAD have long been present in the U.S. and are an important public health issue to be addressed,” said Gornik. “These disparities highlight opportunities for initiatives focused on early disease detection and improving access to effective PAD treatments for people in under-resourced, at-risk communities.”
Detection of PAD in most patients is accomplished through a thorough medical history, physical examination and resting ankle-brachial index (ABI), which measures the ratio of the systolic blood pressure at the ankle to the upper arm. The guideline recommends patient-centered efforts to address health disparities, such as intensified efforts to identify patients in at-risk populations for symptoms and signs of PAD, and equitable access to regular physical examinations including thorough assessment of the legs and feet.
Get with The Guidelines: The PAD National Action Plan
In 2021, the American Heart Association published the PAD National Action Plan, which is endorsed by the American College of Cardiology, that outlines six strategic goals to improve awareness, detection and treatment of PAD nationwide. In the plan, the Association proposed a goal of reducing nontraumatic limb amputation in the U.S. by 20% by 2030.
The guideline writing committee notes that interventions are needed to address the disparity gap in amputation and revascularization procedures among people in diverse racial and ethnic populations and to improve limb and cardiovascular outcomes for all patients with PAD.
“It’s important to recognize the signs and symptoms of PAD and move quickly to initiate treatment to improve outcomes and reduce risks,” said Gornik. “With these updated guidelines, we have the tools necessary to make a positive impact on outcomes in our patients with PAD. Now, we need to work together to implement them as broadly as possible.”
This joint guideline was prepared by a volunteer writing group on behalf of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines, and developed with and endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Podiatric Medical Association, the Association of Black Cardiologists, the Society for Cardiovascular Angiography and Interventions, the Society for Vascular Medicine, the Society for Vascular Nursing, the Society for Vascular Surgery, the Society of Interventional Radiology, and the Vascular & Endovascular Surgery Society. This joint guideline provides the official clinical practice recommendations for the diagnosis and treatment of peripheral artery disease, or PAD.
Reference:
Heather L. Gornik, Herbert D. Aronow, Philip P. Goodney, Shipra Arya, Luke Packard Brewster, Lori Byrd, Venita Chandra, Douglas E. Drachman, Jennifer M. Eaves, Jonathan K. Ehrman, 2024 ACC/AHA/AACVPR/APMA/ABC/SCAI/SVM/SVN/SVS/SIR/VESS Guideline for the Management of Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines, Circulation, https://doi.org/10.1161/CIR.0000000000001251.