Endovascular Thrombectomy Shows Promise Beyond 24 Hours in Vertebrobasilar Occlusion: JAMA
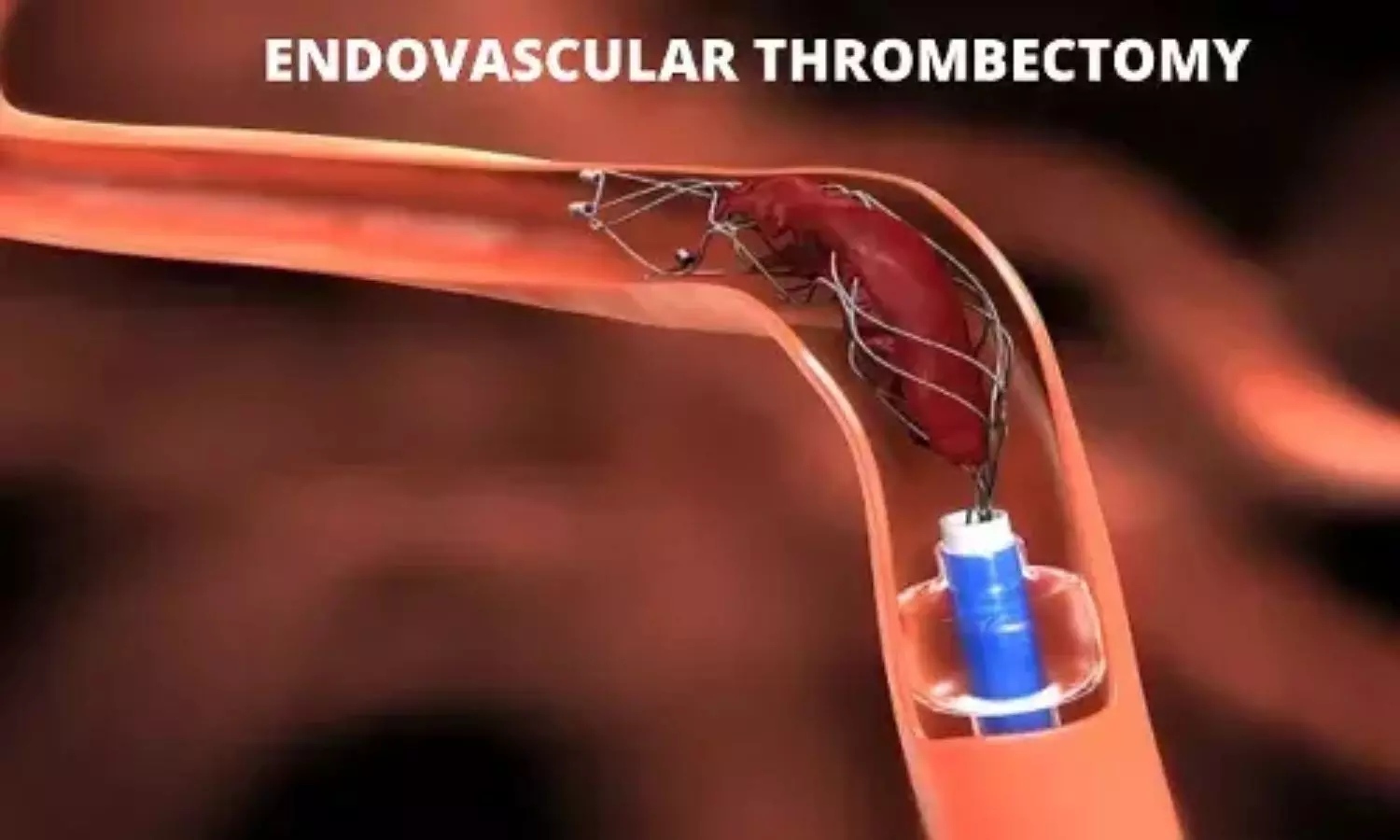
A new study published in the Journal of American Medical Association showed that endovascular thrombectomy may improve functional outcomes in patients with vertebrobasilar artery occlusion presenting after 24 hours, highlighting the need for randomized clinical trials to confirm its efficacy.
For vertebrobasilar artery occlusion (VBAO) that lasts more than 24 hours, the effectiveness and safety of endovascular thrombectomy (EVT) combined with best medical therapy (BMT) are yet unknown. Thus, this study assessed the effects of EVT in patients treated for vertebrobasilar artery blockage more than 24 hours after the last known well time.
The patients from 11 comprehensive stroke centers in China were recruited for this research between 2019 and 2024. Included were eligible individuals whose vertebrobasilar artery occlusions were treated more than 24 hours after the expected occurrence. 2 groups of patients were created: those who had BMT alone and those who received EVT with BMT. Good functional status (modified Rankin Scale score, 0-3) at 90 days was the main result. Ninety-day mortality and symptomatic cerebral bleeding within 24 hours were safety outcomes.
Of the 202 patients with vertebrobasilar occlusion, 101 had EVT with BMT, and 101 received BMT alone. Of these patients, 158 were male [78.2%] and their median [IQR] age was 64.0 [56.2-70.0] years. The median (IQR) period from onset to admission was 48 (24-96) hours, and the median (IQR) posterior circulation Acute Stroke Prognosis Early Computed Tomography Score was 8 (8-9).
71 patients who had EVT with BMT had a greater rate of a favorable functional outcome at 90 days than 71 patients who received BMT alone, according to the primary analysis using propensity score matching (41 patients [57.7%] vs. 32 patients [45.1%]; adjusted risk ratio [aRR], 1.35 [95% CI, 1.02-1.79]).
When comparing EVT with BMT to BMT alone, the death rate was reduced (9 patients [12.7%] vs. 20 patients [28.2%]; aRR, 0.27 [95% CI, 0.08-0.81]); however, there was no statistically significant difference in the rates of symptomatic cerebral bleeding (4 patients [5.6%] vs. 0 patients; P =.13). EVT with BMT showed a similar functional outcome benefit in the inverse probability of treatment weighting analysis (aRR, 1.33 [95% CI, 1.04-1.71]).
Overall, compared to those who got BMT, selected individuals with VBAO who received EVT more than 24 hours after the beginning of symptoms were more likely to have high functional status at three months. For individuals with baseline NIHSS scores of 10 or above, the potential benefit of EVT could be higher.
Source:
Liu, S., Xu, Y., Nguyen, T. N., Gao, F., Xue, Y., Liu, S., Wang, S., Zhang, B., Luo, L., Yue, X., Chang, B., Li, H., Xu, G., Zhang, P., Liu, Y., Cao, Y., Shi, W., Wang, S., Zhao, L., … Wei, M. (2025). Outcomes of endovascular treatment in patients with vertebrobasilar artery occlusion beyond 24 hours. JAMA Network Open, 8(6), e2515526. https://doi.org/10.1001/jamanetworkopen.2025.15526
Powered by WPeMatico