Frailty Significantly Increases Mortality and Complications in PCI Patients, NCDR Registry Study Finds

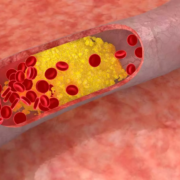
USA: Frailty is common among older patients undergoing percutaneous coronary intervention (PCI) in the United States, with greater frailty linked to significantly higher risks of in-hospital death and procedural complications, according to new findings from the American College of Cardiology’s CathPCI Registry. The study, led by Dr. Benjamin Peterson from the University of Kentucky School of Medicine, was published online in JACC ahead of its June 24, 2025, issue.
The analysis included over 1.3 million patients (mean age 74.6 years; 34% women) aged 65 years or older who underwent PCI between October 2018 and December 2021. Frailty was evaluated using the Canadian Study of Health and Aging Clinical Frailty Scale (CFS), which assesses the ability to perform both basic and instrumental activities of daily living. Patients were classified into four groups: non-frail (CFS 1-2), prefrail (CFS 3-4), frail (CFS 5-6), and severely frail (CFS 7-9).
The key findings were as follows:
- Frailty was widespread among PCI patients, with 67.8% categorized as prefrail, 21.6% as frail, and 2.2% as severely frail.
- The overall in-hospital mortality rate was 2.4%.
- Mortality increased sharply with frailty: 0.5% in nonfrail patients, 1.1% in prefrail, 3.3% in frail, and 20.3% in severely frail patients.
- More than half of all PCIs were performed in patients over 65 years, who account for nearly 80% of PCI-related mortality.
- The study demonstrated a clear gradient of increasing risk tied to frailty status, independent of bedside mortality scores and across various clinical subgroups.
- Among severely frail patients undergoing complex PCI scenarios, mortality rates were 44.2% following cardiac arrest, 51.0% with cardiogenic shock, 46.1% with mechanical circulatory support, 23.9% with chronic total occlusions, 29.6% for left main coronary interventions, and 22.4% with severe calcification.
- The rates of complications, including bleeding, transfusion need, vascular issues, new dialysis initiation, and stroke, consistently rose with increasing frailty severity.
While the authors caution against using these findings to withhold PCI, especially in acute coronary syndromes, they emphasize the importance of incorporating frailty assessment into routine clinical evaluations. “Frailty status, even at the prefrail level, significantly affects procedural risk and should guide shared decision-making,” the authors noted.
In an accompanying editorial, Dr. John A. Dodson and Dr. Ashok Krishnaswami advocate for incorporating frailty screening into routine patient assessment, similar to vital signs, to enhance outcomes for older adults undergoing PCI.
“To meaningfully improve care for older adults, frailty assessment should become a routine part of clinical practice—integrated into every evaluation just as vital signs are,” they wrote.
Reference:
Peterson, B., Kochar, A., Young, R., Senman, B., Rymer, J., Wojdyla, D., … Bhatt, D. L. (2025). Effect of Frailty on In-Hospital Mortality and Complications of PCI: An NCDR Registry Report (Accepted). Journal of the American College of Cardiology, 85(24), 2416–2420. https://doi.org/10.1016/j.jacc.2025.04.027
Powered by WPeMatico