Targeting SBP Below 130 mmHg May Lower Hospitalizations in HFpEF Without Increasing Serious Risks: Meta-analysis

Japan – Targeting a systolic blood pressure (SBP) below 130 mmHg may significantly reduce hospitalizations in patients with heart failure with preserved ejection fraction (HFpEF), a recent systematic review and meta-analysis published in Hypertension Research has revealed. The study, led by Dr. Chisa Matsumoto from the Department of Cardiology at Tokyo Medical University in Fukuoka, Japan, offers important guidance for clinicians ahead of the upcoming Japanese Society of Hypertension 2025 (JSH2025) guidelines.
HFpEF accounts for approximately half of all heart failure cases and remains a clinical challenge, particularly when it comes to optimal blood pressure management. To address this, Dr. Matsumoto and her team systematically reviewed randomized controlled trials (RCTs) published since 2012 that examined the impact of tight BP control, specifically targeting SBP <130 mmHg, on clinical outcomes in HFpEF patients.
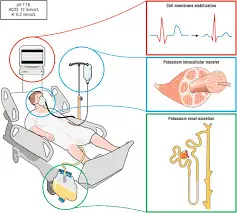
The analysis included six RCTs that collectively assessed various interventions such as mineralocorticoid receptor antagonists, angiotensin receptor-neprilysin inhibitors (ARNIs), intensive BP control strategies, and comprehensive heart failure management approaches. These studies had follow-up periods of at least six months and demonstrated significant BP reduction in intervention groups, achieving SBP below 130 mmHg.
The study led to the following findings:
- Maintaining systolic blood pressure (SBP) below 130 mmHg was associated with a 20% reduction in the risk of heart failure-related hospitalizations (RR: 0.80).
- There was a trend toward reduced all-cause mortality, though it did not reach statistical significance.
- There was a 35% increased risk of hypotension reported (RR: 1.35).
- There was no significant increase in serious adverse events or renal dysfunction, suggesting overall safety was not compromised despite the lower SBP target.
Even though none of the trials were specifically designed to use SBP <130 mmHg as the primary intervention target, the consistent benefits observed across different treatment modalities support the adoption of this threshold in clinical practice for HFpEF patients.
“Based on our findings, we advocate aiming for an SBP under 130 mmHg in HFpEF management, provided that patients are carefully monitored for hypotension,” said Dr. Matsumoto. “Given the heterogeneity of HFpEF, personalized treatment strategies and close clinical observation remain essential.”
The authors call for future trials that directly assess SBP targets and investigate how different antihypertensive agents might be tailored to the complex needs of HFpEF patients.
The study provides timely evidence to inform treatment decisions and guideline development, emphasizing a cautious yet proactive approach to blood pressure control in heart failure care.
Reference:
Matsumoto, C., Nagai, M., Shinohara, K., Morikawa, N., Kai, H., & Arima, H. (2025). Systolic blood pressure lower than 130 mmHg in heart failure with preserved ejection fraction: A systematic review and meta-analysis of clinical outcomes. Hypertension Research, 1-14. https://doi.org/10.1038/s41440-025-02240-w
Powered by WPeMatico