Single-Dose Dexamethasone Lowers Surgical Stress in Laparoscopic Abdominal Surgery: Study
Researchers have found in new research that a single dose of dexamethasone may reduce surgical stress, as reflected by lower C-reactive protein (CRP) levels among patients undergoing laparoscopic abdominal surgery.
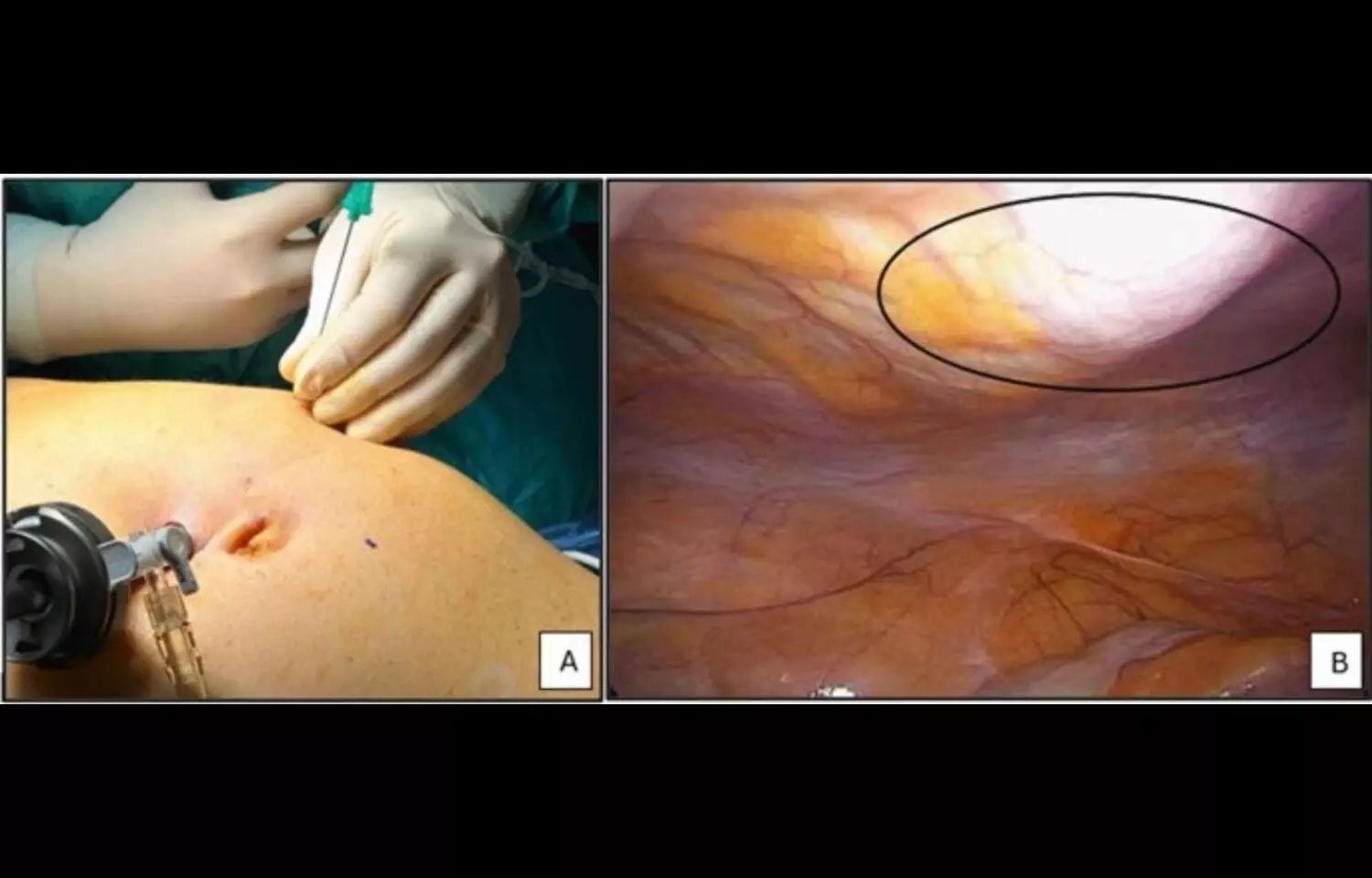
The randomized controlled trial, published in BMC Surgery, investigated whether perioperative dexamethasone could attenuate the systemic inflammatory response triggered by minimally invasive abdominal procedures. Surgical trauma is known to induce inflammatory changes, with CRP serving as a key biomarker of stress and recovery. Researchers evaluated adult patients undergoing elective laparoscopic abdominal surgery, who were randomized to receive either a single intravenous dose of dexamethasone or placebo before surgery. The findings showed that CRP levels were significantly lower in the dexamethasone group compared with controls, suggesting a protective effect against excessive surgical stress. Patients who received dexamethasone also demonstrated more stable postoperative recovery profiles, though the study was not powered to assess broader clinical outcomes such as complication rates or length of hospital stay. Importantly, no major adverse effects were associated with the intervention, reinforcing its potential safety for perioperative use. Authors noted that the results align with existing evidence highlighting the anti-inflammatory and immunomodulatory properties of corticosteroids. By blunting excessive inflammatory activation, dexamethasone could help reduce tissue injury, promote faster recovery, and potentially improve patient comfort. However, the researchers cautioned that further large-scale studies are needed to evaluate long-term benefits, optimal dosing, and impact on hard clinical endpoints such as infection rates or overall morbidity. The study contributes to the growing interest in enhanced recovery strategies in surgery. With laparoscopic techniques already associated with reduced trauma compared to open procedures, the addition of low-dose corticosteroid therapy could further optimize postoperative recovery. Researchers suggested that integrating dexamethasone into perioperative protocols may be a simple, cost-effective approach, though caution remains warranted until more definitive evidence is available.
Keywords: dexamethasone; laparoscopic abdominal surgery; surgical stress; C-reactive protein; randomized controlled trial; perioperative care; corticosteroids; inflammation; recovery; BMC Surgery.
Powered by WPeMatico