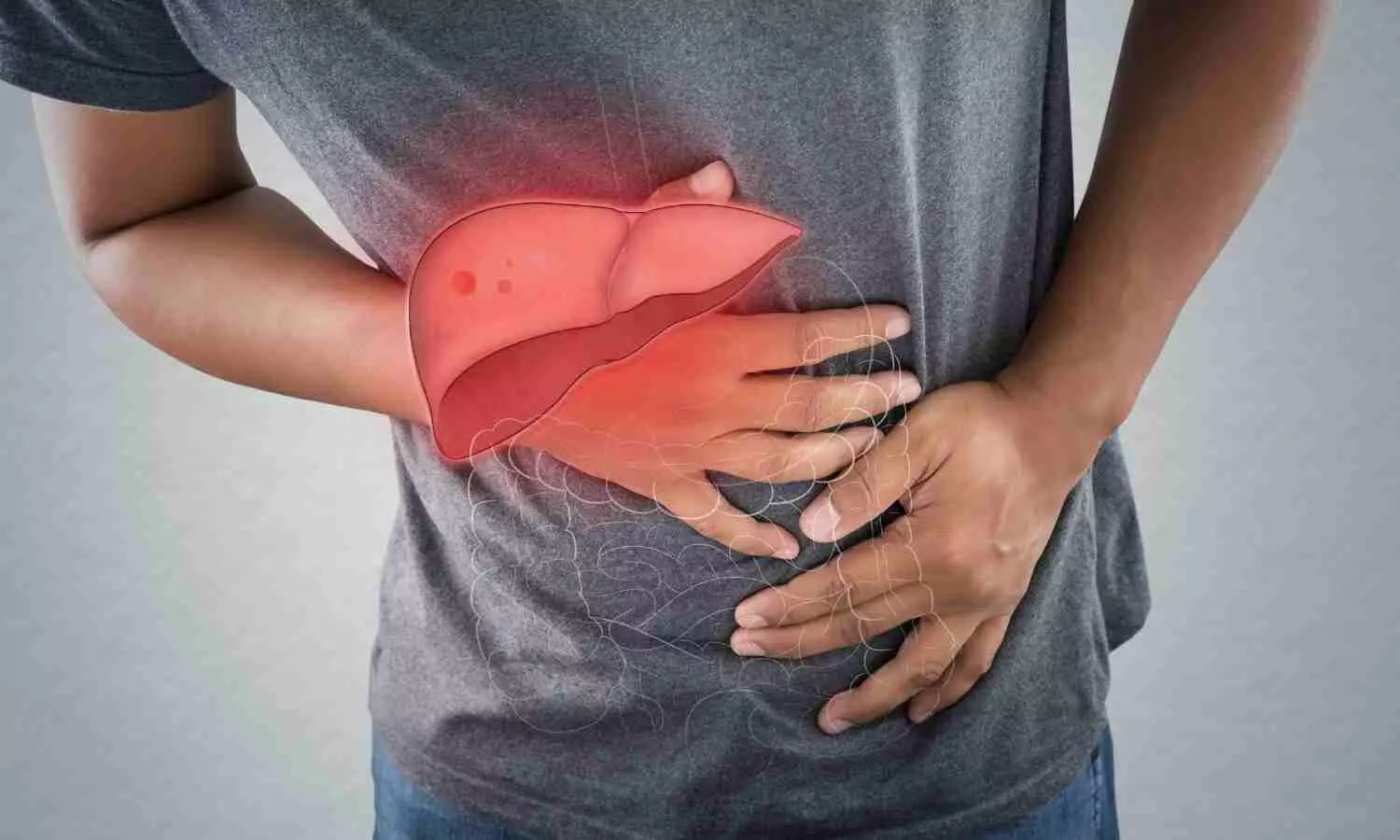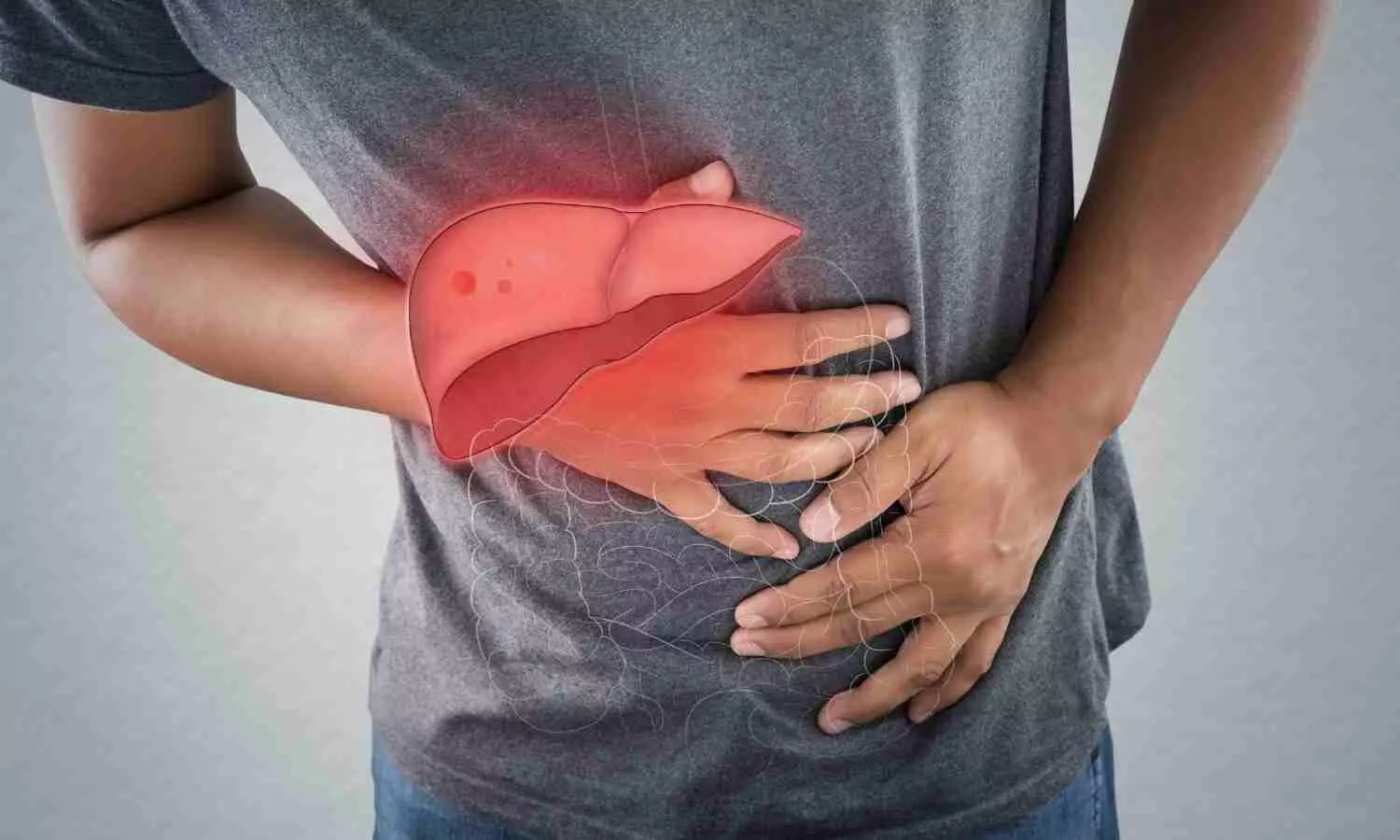
A team from Barcelona discovered that two existing drugs can safely reverse liver fat buildup in MASLD. The combination targets multiple pathways, potentially transforming treatment for fatty liver and related heart risks.
Metabolic dysfunction-associated steatotic liver disease is currently the most widespread liver disorder globally, affecting roughly one in three adults. It occurs when excess fat builds up inside liver cells, leading to serious liver damage and a higher risk of death from cardiovascular disease.
Researchers at the University of Barcelona have now found a promising approach that could change how this condition is treated. Their study, published in Pharmacological Research, reports that two existing drugs, pemafibrate and telmisartan, significantly reduced fat buildup in animal models of metabolic liver disease. The findings also suggest that using these medications together could ease liver damage while lowering related heart and blood vessel complications. Because available treatments for this disease remain very limited, the results point to a potentially safer and more effective therapeutic option.
The research was led by Marta Alegret, a professor at the University of Barcelona’s Faculty of Pharmacy and Food Sciences, and a member of the Institute of Biomedicine of the UB (IBUB) and the CIBER Area for Physiopathology of Obesity and Nutrition (CIBEROBN). The work was conducted in collaboration with scientists from the Santa Creu i Sant Pau Hospital Research Institute, the Hospital Clínic de Barcelona, the CIBER Area for Cardiovascular Diseases (CIBERCV), and Uppsala University (Sweden).
Drug repurposing, a promising and cost-effective strategy
To date, most new experimental compounds developed for metabolic dysfunction-associated steatotic liver disease (MASLD) — formerly known as fatty liver disease — have failed during clinical trials, often because of safety concerns. This has turned attention toward drug repurposing, a strategy that explores new uses for medications already proven to be safe in humans. Such an approach is not only faster and more affordable but also particularly valuable for treating the early, often symptom-free stages of MASLD.
“We have focused on these phases with the aim of preventing the disease from progressing to more severe stages. But for a drug to be used in these early stages, it must have a good safety profile in humans,” explains Marta Alegret. “That is why we have studied drugs already on the market for other pathologies, which have been shown to be very safe and could have a potential benefit in the treatment of MASLD,” she adds.
In this study, the team evaluated the potential of two approved medications, given separately and together: a lipid-lowering agent (pemafibrate) and an antihypertensive drug (telmisartan). The first is marketed only in Japan, while the second is widely used for high blood pressure. Both are prescribed to reduce cardiovascular risk. “Mortality from cardiovascular causes is significant in patients with MASLD, and often these patients also have these two risk factors together,” Alegret stresses.
Zebrafish larvae, an alternative model for studying the disease
To confirm the efficacy of the drugs and explore their mechanism of action, the researchers have applied them to a rat model of the disease and, subsequently, to a zebrafish larval model. “In recent years, zebrafish have emerged as an interesting alternative model that facilitates the study of the pathophysiology of MASLD and the evaluation of treatments. These are simpler and cheaper models that allow results to be obtained more quickly and which, although they are not identical to humans, have a carbohydrate/lipid metabolism and liver physiology similar to those of mammals,” says the UB professor.
The results show that the combination of the two drugs reverses the fat accumulation in the liver induced by a diet high in fat and fructose. In addition, in the rat model, the combined administration of half a dose of pemafibrate and half a dose of telmisartan was found to be as effective as a full dose of either drug in reducing fat accumulation. “Combination therapy with drugs acting on different pathogenic pathways may be a better strategy than monotherapy, thanks to possible synergistic effects and reduced toxicity related to the use of lower doses of each drug,” Alegret points out.
The combination of these two drugs would be beneficial not only for liver disease, but also because “it lowers blood pressure and cholesterol levels, and all this would result in a lower cardiovascular risk,” she stresses.
Different lipid-lowering mechanisms The study also found that each drug works by different mechanisms and describes, for the first time, the key role of the PCK1 protein in telmisartan-derived hepatic lipid lowering. “Telmisartan is a drug that has been used in other models of MASLD, but mostly in more advanced stages of the disease, and its beneficial effects have been attributed mainly to anti-inflammatory and anti-fibrotic effects. But in the early stages of the disease there is no inflammation or fibrosis yet, only lipid accumulation,” explains the researcher.
Researchers have now found that the amount of PCK1 protein in the livers of MASLD animals was reduced and that treatment with telmisartan restored its levels to normal. “This increase in PCK1 diverts the flux of metabolites from lipid synthesis to glucose synthesis. This increase in glucose production could be negative if the glucose were exported and accumulated in the blood, as it could lead to diabetes, but we have noticed that this is not the case,” says the UB professor.
Still far from clinical application
Despite these promising results, the researchers point out that, as this is a study using animal models, they are still far from patients. “In order to be translated into a treatment for MASLD patients, clinical studies would be needed to show that the benefits observed in animal models also occur in humans,” says Alegret. In any case, the results raise new questions, such as whether the drugs will be equally effective in more advanced stages of the disease, when fibrosis is present. The research team is therefore already working on new studies in animal models of diet-induced liver fibrosis. “In addition, we will develop a dual model involving liver fibrosis and cardiovascular disease to see if the beneficial action is observed not only in the liver, but also in the reduction of atherosclerosis,” he concludes.
Reference:
Roger Bentanachs, Patricia Ramírez-Carrasco, Bianca Braster, Anastasia Emmanouilidou, Endrina Mujica, Maite Rodrigo-Calvo, Cristina Rodríguez, Núria Roglans, Marcel den Hoed, Juan C. Laguna, Marta Alegret. Telmisartan reverses hepatic steatosis via PCK1 upregulation: A novel PPAR-independent mechanism in experimental models of MASLD. Pharmacological Research, 2025; 218: 107860 DOI: 10.1016/j.phrs.2025.107860