Costoclavicular Technique for Perineural Catheter Insertion in brachial plexus block effectively controls pain after upper limb orthopedic procedures: Study

Even with advancements in perioperative pain management, patients who undergo upper limb orthopaedic surgeries often experience moderate pain once the effects of their initial nerve block wear off. Administering continuous perineural infusion following a single injection enhances postoperative pain relief and reduces the need for additional pain medication. Recent study compared the postoperative local anesthetic (LA) consumption and other outcomes between two different techniques (costoclavicular and lateral sagittal) of inserting a perineural catheter for regional analgesia after upper limb orthopedic surgery.
Patient Selection and Perineural Catheter Technique
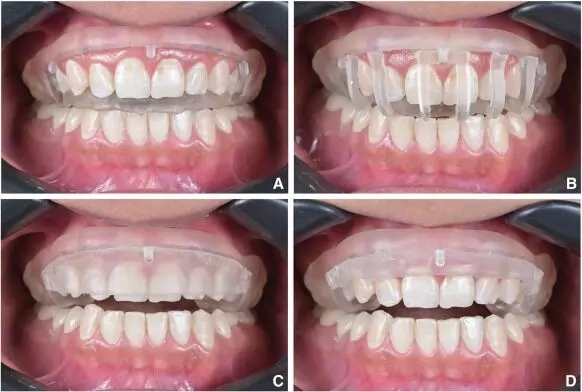
Eighty patients undergoing upper limb orthopedic surgery were randomly assigned to receive a perineural catheter via either the costoclavicular (CC) technique (Group CC) or the lateral sagittal (LS) technique (Group LS). Postoperatively, all patients received patient-controlled regional analgesia with 0.125% bupivacaine.
Results
The primary outcome was the 24-hour LA consumption. The results showed that patients in Group CC required significantly less LA over 24 hours compared to Group LS (83.35 ml vs 121.40 ml, p<0.001). Patients in Group CC also took a longer time to activate the patient-controlled analgesia (p=0.003) and reported better satisfaction scores (p=0.001) compared to Group LS. Pain scores were similar between the two groups.
Complications
One patient in Group CC experienced transient paresthesia which resolved on removal of the catheter. There were no other complications like vascular injury or LA toxicity in either group.
Conclusion
The study concluded that patients receiving postoperative analgesia via the costoclavicular perineural catheter technique required less 24-hour local anesthetic and reported better satisfaction compared to the lateral sagittal technique. The compact and consistent anatomy of the brachial plexus cords in the costoclavicular space likely contributed to the improved analgesic efficacy of this approach.
This randomized trial provides evidence that the costoclavicular technique for inserting perineural catheters can be an effective method for providing prolonged postoperative analgesia after upper limb orthopedic procedures.
Key Points –
The key points from the provided research paper are:
1. The study compared the postoperative local anesthetic (LA) consumption and other outcomes between two different techniques (costoclavicular and lateral sagittal) of inserting a perineural catheter for regional analgesia after upper limb orthopedic surgery.
2. Eighty patients were randomly assigned to receive a perineural catheter via either the costoclavicular (CC) technique (Group CC) or the lateral sagittal (LS) technique (Group LS), and all patients received patient-controlled regional analgesia with 0.125% bupivacaine postoperatively.
3. The primary outcome was the 24-hour LA consumption, and the results showed that patients in Group CC required significantly less LA over 24 hours compared to Group LS (83.35 ml vs 121.40 ml, p<0.001). Patients in Group CC also took a longer time to activate the patient-controlled analgesia (p=0.003) and reported better satisfaction scores (p=0.001) compared to Group LS.
4. Pain scores were similar between the two groups.
5. One patient in Group CC experienced transient paresthesia which resolved on removal of the catheter, and there were no other complications like vascular injury or LA toxicity in either group.
6. The study concluded that the costoclavicular perineural catheter technique can be an effective method for providing prolonged postoperative analgesia after upper limb orthopedic procedures, likely due to the compact and consistent anatomy of the brachial plexus cords in the costoclavicular space.
Reference –
Mondal S, Sinha C, Kumari P, Kumar A, Kumar A, Agarwal P. Costoclavicular versus lateral sagittal infraclavicular brachial plexus block for postoperative analgesia in patients undergoing upper limb orthopaedic surgery: A randomized controlled trial. Indian J Anaesth 2024;68:693‑8.
Powered by WPeMatico