Laparoscopic Supracervical has Lower Postoperative Risks in Uterine Fibroid Surgery vs Total Hysterectomy: Study
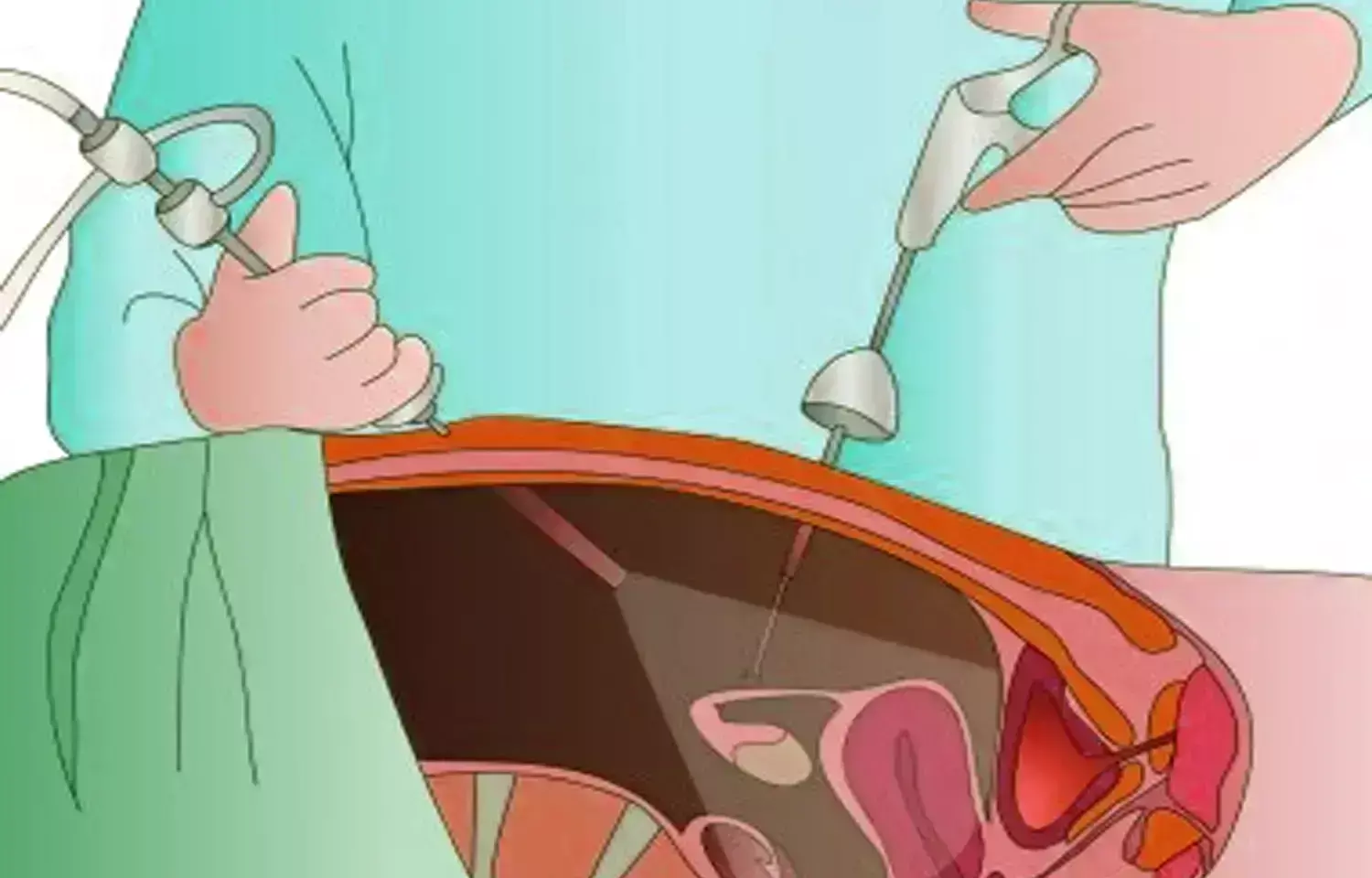
Researchers have found in a new study that Laparoscopic supracervical hysterectomy was linked to a lower risk of short-term postoperative complications compared to total laparoscopic hysterectomy in patients with uterine fibroids, supporting its consideration during shared decision-making for minimally invasive surgery.
Uterine fibroids are the most common indication for benign hysterectomy in the United States, but data regarding the association between hysterectomy type and outcomes for this indication are lacking.This study aimed to describe the rate and odds of short-term (30 days) postoperative complications between patients who underwent minimally invasive total laparoscopic hysterectomy and those who underwent laparoscopic supracervical hysterectomy for uterine fibroids. This was a cohort study of prospectively collected data from the American College of Surgeons National Surgical Quality Improvement Program database from 2012 to 2020. The characteristics of women who underwent total laparoscopic hysterectomy and those who underwent laparoscopic supracervical hysterectomy for uterine fibroids were identified. In addition, the risk factors associated with the occurrence of 30-day postoperative complications, defined according to the Clavien-Dindo classification, were identified. Multivariate regression analysis, including age, body mass index, race, comorbidities, American Society of Anesthesiologists classification, uterine weight, and concomitant procedures, was performed to identify the adjusted odds of postoperative complications. The co-primary outcomes were (1) the risk of a composite of any postoperative complications and (2) the risk of major postoperative complications according to surgical type.Results: Overall, 44,413 patients underwent minimally invasive total laparoscopic hysterectomy, and 6383 patients underwent laparoscopic supracervical hysterectomy. The operative time was shorter in the total laparoscopic hysterectomy group than in the laparoscopic supracervical hysterectomy group (143.0 vs 150.6 minutes, respectively; P < .001). In addition, the proportion of uterine weight of >250 g was lower in the total laparoscopic hysterectomy group than in the laparoscopic supracervical hysterectomy group (39.4% vs 45.1%, respectively; P < .001). The rates of any and major complications were higher in the total laparoscopic hysterectomy group than in the laparoscopic supracervical hysterectomy group (any complications: 6.6% vs 5.3%, respectively; P < .001; major complications: 2.7% vs 1.6%, respectively; P < .001), whereas the rates of minor complications were comparable in both groups (4.4% vs 4.1%, respectively; P = .309). In multivariate regression analysis, laparoscopic supracervical hysterectomy was independently associated with a lower risk of any (adjusted odds ratio, 0.79; 95% confidence interval, 0.70–0.88) and major (adjusted odds ratio, 0.55; 95% confidence interval, 0.44–0.69) complications than total laparoscopic hysterectomy. Laparoscopic supracervical hysterectomy was associated with a lower risk of short-term postoperative complications in patients with uterine fibroids than total laparoscopic hysterectomy. Our findings can aid in shared decision-making before minimally invasive hysterectomy for uterine fibroids.
Reference:
Raanan Meyer, Kacey M. Hamilton, Rebecca J. Schneyer, Gabriel Levin, Mireille D. Truong, Kelly N. Wright, Matthew T. Siedhoff. Short-term outcomes of minimally invasive total vs supracervical hysterectomy for uterine fibroids: a National Surgical Quality Improvement Program study. American Journal of Obstetrics and Gynecology, Volume 232, Issue 4, 2025, Pages 377.e1-377.e10, ISSN 0002-9378, https://doi.org/10.1016/j.ajog.2024.10.006. (https://www.sciencedirect.com/science/article/pii/S0002937824010548)
Keywords:
Laparoscopic, Supracervical, Lower, Postoperative, Risks, Uterine, Fibroid, Surgery, Total Hysterectomy, Study , American Journal of Obstetrics and Gynecology, Raanan Meyer, Kacey M. Hamilton, Rebecca J. Schneyer, Gabriel Levin, Mireille D. Truong, Kelly N. Wright, Matthew T. Siedhoff
