High-intensity focused ultrasound with endometrial thermal balloon ablation efficacious and safe for adenomyosis: Study
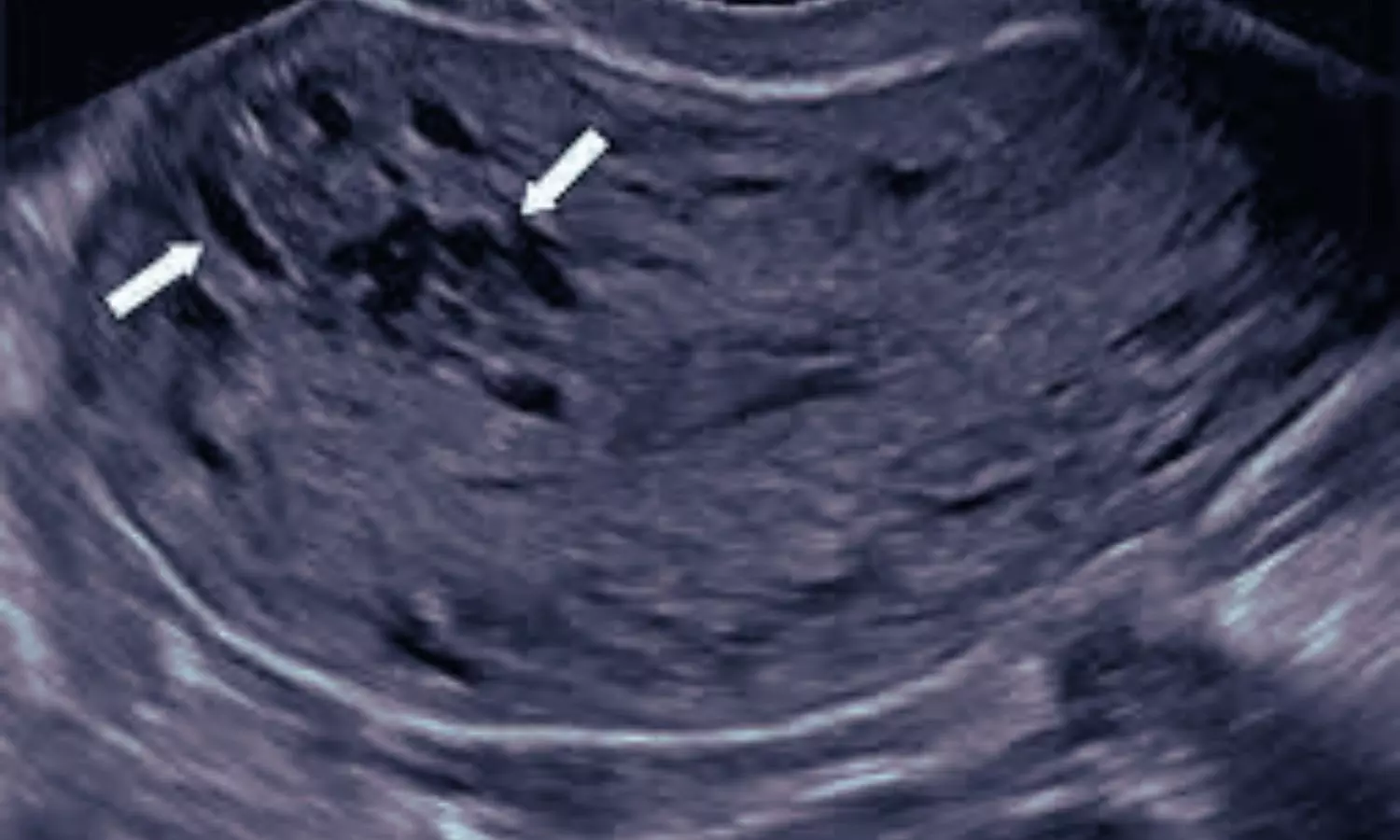
Adenomyosis is a condition characterized by the invasion of
endometrial glands and stroma into the myometrium. Its primary clinical
symptoms include excessive menstruation, dysmenorrhea, and infertility, which
severely affect patients’ quality of life and overall wellbeing. Drug therapy,
interventional therapy and uterus-preserving surgery have the disadvantages of
timeliness, recurrence and trauma. Total hysterectomy, a radical treatment
option, is typically recommended for older patients who have no reproductive
needs and have failed to respond to medication or conservative treatments.
However, hysterectomy can cause significant psychological and physiological
stress, making it a last-resort option in clinical practice. This highlights
the urgent need to develop effective long-term management strategies for
patients with adenomyosis who have experienced multiple treatment failures but
wish to preserve their uterus.
High-intensity focused ultrasound (HIFU) ablation, a
minimally invasive treatment, has shown promising short-term improvements in
dysmenorrhea and menorrhagia symptoms in patients with adenomyosis. However, it
has been found to be less effective in controlling menorrhagia over the long
term. Compared with HIFU alone, the combination of HIFU with
gonadotropin-releasing hormone agonist (GnRH-a) and levonorgestrel-releasing
intrauterine system (LNG-IUS) (HIFU + GnRH-a + LNG-IUS) has demonstrated
enhanced long-term efficacy and a lower recurrence rate. Nonetheless, the use
of hormonal medications such as GnRH-a and LNG-IUS is associated with various
adverse effects, and patient compliance tends to be poor.
Endometrial thermal balloon ablation (TBEA) is a minimally
invasive procedure that provides a simple and effective treatment option for
patients with adenomyosis-related menorrhagia. However, since TBEA cannot
target deep myometrial lesions and causes irreversible damage to the
endometrium, its application in adenomyosis treatment is controversial and
unsuitable for women with fertility needs. HIFU possesses unique
characteristics of directionality, penetration, and focus, enabling the precise
targeting of high-energy ultrasound waves to lesions within the myometrium for
effective ablation of deep-seated lesions. This property compensates for the
limitations of TBEA in addressing myometrial lesions. Theoretically, combining
HIFU and TBEA offers complementary advantages, providing an optimized treatment
strategy for adenomyosis patients with menorrhagia who do not require fertility
preservation, thereby significantly enhancing therapeutic efficacy.
Currently, there is a lack of clinical research
internationally on the combined application of HIFU and TBEA for the treatment of
adeno myosis. Since 2021, authors’ research team has conducted a clinical
cohort study on HIFU combined with TBEA for adenomyosis. Based on this
foundation, this study aimed to conduct a retrospective analysis to evaluate
the efficacy and safety of HIFU combined with TBEA in comparison with
standalone HIFU and HIFU combined with GnRH-a and LNG-IUS, to alleviate
adenomyosis-related hypermenorrhagia, thereby providing scientific evidence for
the optimization of adenomyosis treatment strategies.
This retrospective cohort study included 120 patients
diagnosed with adenomyosis-related hyper menorrhagia. Patients were divided
into three groups: the HIFU combined with TBEA group (HIFU + TBEA, 34 cases),
the HIFU combined with gonadotropin-releasing hormone agonist and intrauterine
levonorgestrel intrauterine system (HIFU + GnRH-a + LNG-IUS, 51 cases) group
and the HIFU (35 cases) group. Efficacy and safety were assessed using the
pictorial blood loss assessment chart (PBAC), dysmenorrhea scores evaluated by
the Numerical Rating Scale (NRS), quality of life measured by the Uterine
Fibroid Symptom and Quality of Life scale (UFS-QOL), reintervention rates,
success rates, satisfaction, and adverse effects at pretreatment and 1, 3, 6,
9, and 12 months posttreatment.
The HIFU + TBEA group showed significantly greater
reductions in PBAC scores at 6, 9, and 12 months compared to the HIFU + GnRH-a
+ LNG-IUS group, and consistently lower scores than the HIFU group at all
follow-up points. No significant differences in NRS scores or reintervention
rates were observed between groups. Additionally, the HIFU + TBEA group
reported higher UFS-QOL scores at 6 and 12 months posttreatment and greater
satisfaction at 12 months posttreatment. Its success rate exceeded that of the
HIFU group but was comparable to the HIFU + GnRH-a + LNG-IUS group. Serious
adverse reactions were rare across all groups.
HIFU is a noninvasive, repeatable treatment for adenomyosis
that ablates adenomyotic lesions. While effective in the short term, its
longterm efficacy as a standalone treatment is limited. A study of 1,982
patients showed that combining HIFU with GnRH-a and LNG-IUS achieved the best
long-term results. This study adopts the HIFU + GnRH-a + LNG-IUS combination as
the control group to optimize clinical efficacy. However, despite its effectiveness,
this combination therapy is associated with a higher incidence of adverse
effects. TBEA is a minimally invasive procedure that reduces abnormal uterine
bleeding by thermally ablating the endometrial layer, inducing coagulation necrosis
and fibrosis. While effective in reducing bleeding with minimal side effects,
TBEA cannot ablate the myometrium and is less effective for dysmenorrhea.
Moreover, its irreversible endometrial damage makes it unsuitable for patients
desiring fertility. Standalone TBEA is not a first-line treatment for
adenomyosis. This study pioneers combining HIFU’s targeted myometrial ablation
with TBEA’s endometrial-specific capabilities, comparing it to HIFU + GnRH-a +
LNG-IUS and standalone HIFU to evaluate its clinical value in treating
adenomyosis-related hypermenorrhagia.
HIFU combined with TBEA offers significant advantages in
treating adenomyosis with heavy menstrual bleeding. This approach not only
improves symptoms of dysmenorrhea but also achieves high patient satisfaction
rates and substantial enhancements in quality of life. As a novel clinical
reference, this treatment provides an effective option for managing
adenomyosis-related hypermenorrhagia in patients without fertility preservation
requirements.
Source: Z. Jin et al.; European Journal of Obstetrics &
Gynecology and Reproductive Biology 307 (2025) 134–141
