First Reported Case Links PreserFlo MicroShunt Surgery to RPE Tear and Serous Retinal Detachment
Japan: A recent case report published in BMC Ophthalmology by Ayako Sadahide and colleagues from the Department of Ophthalmology and Visual Science, Hiroshima University Hospital, Japan, documents the first known instance of serous retinal detachment (SRD) accompanied by a retinal pigment epithelium (RPE) tear following PreserFlo MicroShunt (PMS) surgery. The minimally invasive glaucoma device is designed to reduce intraocular pressure (IOP) with fewer complications than traditional filtration surgeries. However, this case highlights the need for careful postoperative monitoring, especially in patients with predisposing ocular and systemic factors.
The report describes a 53-year-old man with ocular hypertension and a history of cataract surgery with intraocular lens (IOL) fixation who underwent PMS due to uncontrolled IOP. The patient also had a history of atopic dermatitis and prolonged use of potent topical steroids, factors suspected to compromise choroidal microcirculation and RPE integrity.
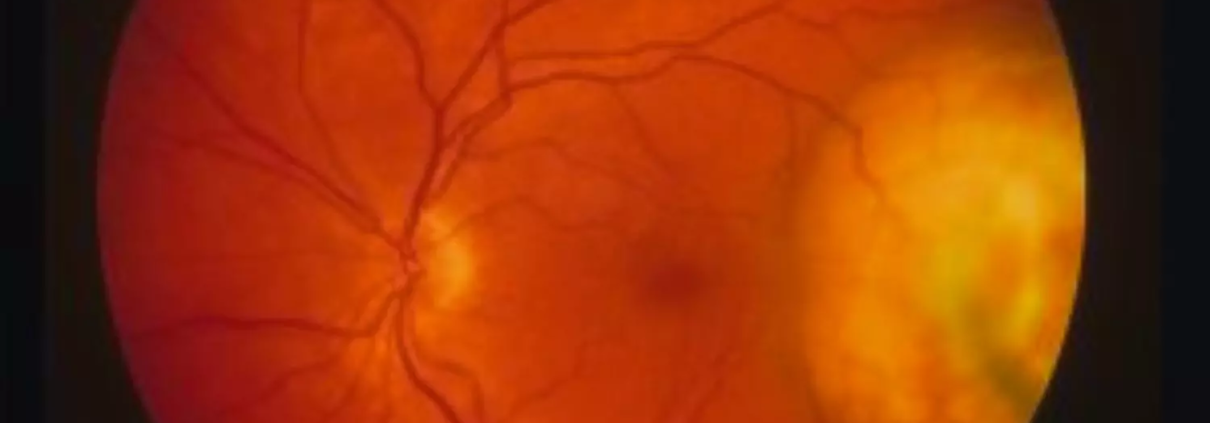
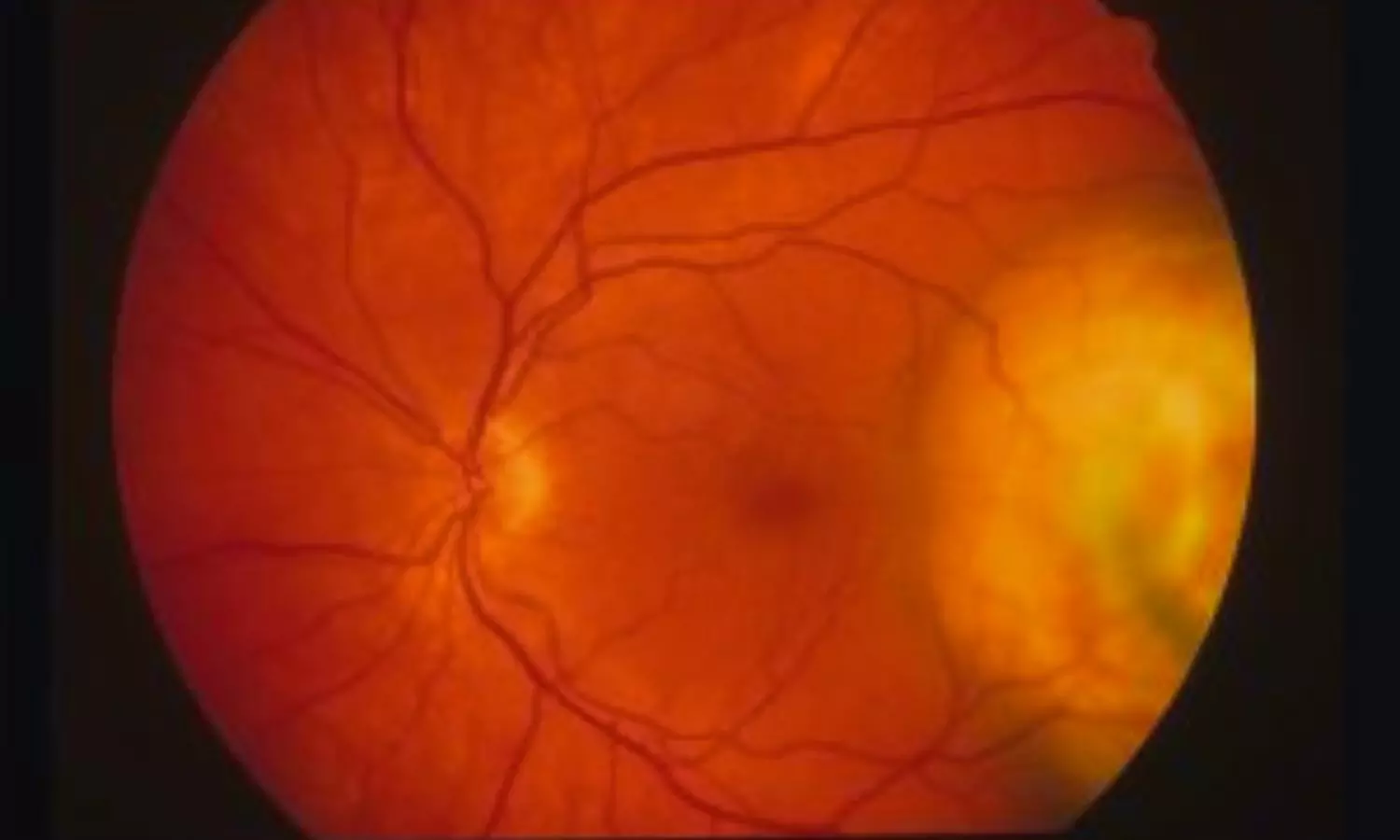
Initially, the surgery appeared successful, lowering IOP from 42 mmHg to 10 mmHg on the first postoperative day. However, within days, the patient developed ciliochoroidal detachment (CD), a known complication of glaucoma surgery under hypotonic conditions. Despite conservative management with atropine and topical steroids, the condition progressed. By one month post-surgery, the patient’s vision dropped to 20/500, and bullous serous retinal detachment involving the macula was noted. Imaging revealed extensive RPE tears in the inferior regions of the retina.
To prevent further deterioration, surgeons performed scleral drainage and pars plana vitrectomy with sulfur hexafluoride (SF6) gas tamponade. The procedure successfully elevated IOP and led to the resolution of the detachment. Postoperatively, the patient’s IOP stabilized in the mid-teens with no recurrence of SRD, though postoperative angiography confirmed the presence of window defects consistent with RPE tears.
According to the authors, the case emphasizes that not only absolute postoperative hypotony but also a rapid and significant drop in IOP can disturb choroidal blood flow and compromise RPE function, especially in eyes with structural vulnerabilities. The findings suggest that eyes with exfoliation syndrome, long-term steroid exposure, or pre-existing choroidal circulatory compromise may be particularly susceptible to such complications.
Previous reports of SRD and RPE tears have been associated with conventional glaucoma filtration surgeries, but until now, none have been linked to PMS. The authors propose that the dramatic pressure change, combined with a fragile RPE due to chronic steroid use and atopic dermatitis, likely triggered the sequence of CD, RPE tear, and SRD in this case.
The report highlights the importance of individualized surgical planning and vigilant postoperative monitoring in glaucoma patients, especially when risk factors for RPE fragility exist. Early recognition of choroidal detachment and prompt IOP-elevating interventions may be critical in preventing vision-threatening outcomes.
“The study emphasizes that while PMS is generally safe and effective, clinicians should be aware of this rare but serious complication. Further research is needed to better understand the underlying mechanisms and to establish preventive strategies for high-risk patients undergoing minimally invasive glaucoma surgery,” the authors concluded.
Reference:
Sadahide, A., Harada, Y., Sakaguchi, H. et al. Serous retinal detachment with retinal pigment epithelium tear after PreserFlo MicroShunt surgery: a case report. BMC Ophthalmol 25, 424 (2025). https://doi.org/10.1186/s12886-025-04259-6