Mid-Trimester Blood Test and Treatment Bundle may Reduce Preterm Birth Risks: Study
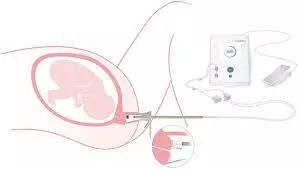
According to a new research mid-trimester blood test successfully identified average-risk women at risk for preterm birth. Researchers found that a treatment bundle, including progesterone and low-dose aspirin, significantly reduced neonatal morbidity and hospital stay compared to usual care. Presented at The Pregnancy Meeting, the study showed that when paired with a three-step treatment bundle, the predictive blood test markedly improved neonatal outcomes.
Obstetric advances have had limited impact on preterm birth (PTB) rates and neonatal outcomes. We assessed outcomes in a cohort of average risk singleton pregnancies using biomarker-based PTB risk stratification, followed by interventions for those identified at higher risk. This randomized controlled trial enrolled 5,018 singleton pregnancies at 19 U.S. centers from 2020-2023. Individuals with prior PTB, short cervix, severe maternal conditions, or known genetic/fetal anomalies were excluded. We measured the ratio of maternal circulating insulin-like growth factor-binding protein 4 to sex hormone-binding globulin between 18w0d and 20w6d, with participants randomized 1:1. The control arm, blinded to test results, received usual care, while the prevention arm received test results. Prevention arm participants identified as high-risk were offered a regimen of daily vaginal progesterone, low-dose aspirin, and weekly nursing calls. Lower-risk participants in the prevention arm received usual care. Follow-up continued through delivery and neonatal discharge. The prespecified modified intent-to-treat (mITT) analysis included the control group, prevention arm low-risk participants, and high-risk participants who consented to intervention by 24 weeks, while excluding those hospitalized with COVID-19. Primary outcomes included neonatal length of stay (NNLOS) and a composite morbidity index (NMI). A planned intent-to-treat (ITT) analysis assessed multiple neonatal outcomes. Results: Baseline characteristics did not differ between arms. mITT analysis of co-primary outcomes (Table 1) showed significantly decreased NMI and NNLOS in the prevention arm. The ITT analysis displayed significant reductions in NMI (20%), NNLOS (8%), neonatal intensive care unit (NICU) length of stay (6%), and NICU admission (20%). In an average risk singleton population, a mid-trimester blood test identified pregnancies at higher PTB risk, and implementing the treatment bundle significantly reduced neonatal morbidity and hospital stay compared to usual care.
Reference:
Iriye, B. K., O’Brien, J., Ennen, C. S., Barrilleaux, P., Berkin, J., Palatnik, A., Son, M., Gyamfi-Bannerman, C., McDonald, M., Markenson, G., Sciscione, A. C., Biggio, J. R., Wolf, S., Sullivan, S., Walker, M., Shahbaba, B., & Pound, S. P. (2025, January 31). Neonatal impact of prematurity risk biomarker screening with targeted interventions: A multicenter randomized controlled trial [Conference presentation]. Aurora Ballroom, Lobby Level, Hera Women’s Health, Las Vegas, NV, United States.
Keywords:
Mid-Trimester, Blood Test, Treatment, Bundle, Reduce, Preterm, Birth Risks, Iriye, B. K., O’Brien, J., Ennen, C. S., Barrilleaux, P., Berkin, J., Palatnik, A., Son, M., Gyamfi-Bannerman, C., McDonald, M., Markenson, G., Sciscione, A. C., Biggio, J. R., Wolf, S., Sullivan, S., Walker, M., Shahbaba, B., & Pound, S. P.
