Study explores ‘social norms’ of distracted driving among teens
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
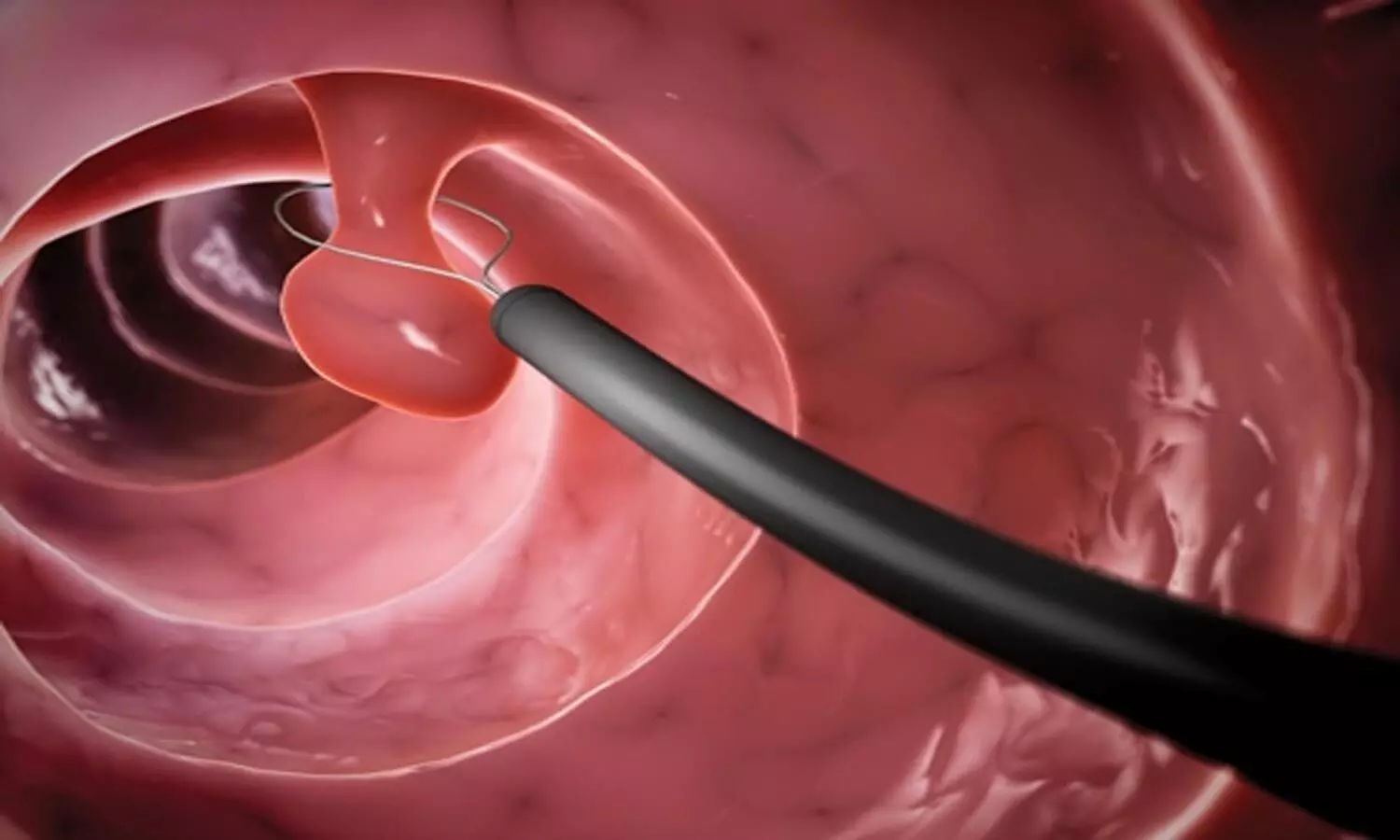
Fasting and bowel preparation before colonoscopy can lead to intravascular volume depletion, but rigorous assessment of its clinical implications is limited. Recent prospective cohort study was conducted to evaluate the relationship between intravascular volume status and hypotension during propofol sedation for elective colonoscopy. The cohort included adult patients undergoing colonoscopy following polyethylene glycol (PEG) bowel preparation. Using a combination of transthoracic echocardiography (TTE) and ClearSight noninvasive monitoring, the study aimed to assess pre-procedural volume status and monitor intraprocedural hemodynamics.
Patient Analysis
Among the 99 patients analyzed, 32% exhibited signs of intravascular volume depletion based on TTE assessments following a passive leg-raising test. The study observed inadequate agreement between TTE and ClearSight measurements of stroke volume at baseline and post-leg raising, casting doubt on the reliability of the noninvasive monitor alone in determining volume status. Notably, significant intraprocedural hypotension, defined as a mean arterial pressure below 60 mm Hg, was more prevalent in patients identified as fluid-responsive compared to those who were normovolemic (48% vs. 21%, respectively).
Demographic Insights
The lack of significant association between demographic variables (age, ASA status, antihypertensive therapy) and fluid responsiveness suggests that other factors may be influencing intravascular depletion. Fasting durations for fluids and food averaged 9 hours and 25 hours, respectively, which aligns with established guidelines, yet the risks associated with fasting and required bowel preparation persist.
Monitoring Implications
The study emphasizes that while individuals undergoing colonoscopy may frequently display signs of fluid responsiveness, their hemodynamic stability remains questionable, especially under sedation’s influence. Propofol’s vasodilatory effects amplify this concern, suggesting a need for vigilant monitoring during procedures. Though current recommendations encourage intravenous fluid administration as a preventive strategy against hypotension, its efficacy continues to be debated.
Conclusions and Future Directions
Overall, the findings underscore a critical gap in understanding the clinical impacts of bowel preparation-induced volume depletion during colonoscopy. The study suggests a need for further investigation into the optimal management of intravascular volume status pre-procedurally and the overall necessity of advanced monitoring approaches in outpatient endoscopic settings to mitigate adverse outcomes.
Key Points
– A prospective cohort study assessed the impact of fasting and bowel preparation on intravascular volume status and hypotension during propofol sedation in elective colonoscopy, revealing that volume depletion may lead to significant hemodynamic instability.
– Transthoracic echocardiography (TTE) indicated that 32% of the 99 patients studied exhibited signs of intravascular volume depletion after a passive leg-raising test; however, there was a notable lack of agreement between TTE and ClearSight noninvasive monitoring regarding stroke volume measurements, raising concerns about the latter’s reliability.
– Patients identified as fluid-responsive experienced a higher incidence of significant intraprocedural hypotension compared to those classified as normovolemic (48% vs. 21%), demonstrating the potential risks associated with inadequate volume status during sedation.
– Demographic factors such as age, ASA status, and antihypertensive medication use did not correlate with fluid responsiveness, indicating the involvement of other unidentified elements in intravascular depletion.
– The study highlighted the necessity of ongoing monitoring during colonoscopies, particularly under propofol sedation, due to the anesthetic’s vasodilatory effects which can exacerbate hypotensive episodes, despite existing guidelines recommending preventive intravenous fluid administration.
– Findings point to an urgent need for enhanced understanding and management strategies for intravascular volume status prior to procedures, advocating for the exploration of advanced monitoring techniques in outpatient endoscopic environments to minimize the risk of adverse events.
Reference –
Allen, M.L., Kluger, M., Schneider, F. et al. Fluid responsiveness and hypotension in patients undergoing propofol-based sedation for colonoscopy following bowel preparation: a prospective cohort study. Can J Anesth/J Can Anesth 72, 529–539 (2025). https://doi.org/10.1007/s12630-025-02939-x
Powered by WPeMatico

Researchers at Tohoku University have discovered that an oral drug called MA-5 can improve both heart and muscle problems in Barth syndrome, a rare genetic disorder affecting 1 in 300,000 births worldwide with no current cure.
Barth syndrome is caused by mutations in the TAZ gene that leave patients-mostly young boys-with weakened hearts, muscle fatigue, and increased rates of infection. Many require heart transplants, and current treatments only manage symptoms without addressing the underlying cause.
The research team, led by Professors Takaaki Abe, and Takafumi Toyohara, and first author Yoshiyasu Tongu, tested MA-5 on cells from four Barth syndrome patients and in fruit fly (Drosophila) models of the disease. Published in The FASEB Journal on June 21, 2025, their findings reveal that MA-5 boosted cellular energy (ATP) production by up to 50% and protected cells from oxidative stress-induced death.
“What excites us most is that MA-5 works by targeting the fundamental problem in Barth syndrome-defective energy production in mitochondria,” explains Abe. “Unlike current treatments that only manage symptoms, MA-5 actually improves the root cause of how cells generate energy.”
MA-5 was chosen as a treatment because it enhances interactions between two crucial mitochondrial proteins-mitofilin and ATP synthase-leading to more efficient energy production. As such, this mechanism directly addresses the cause of cellular dysfunction in Barth syndrome.
In human muscle cells derived from Barth syndrome iPS cell models, MA-5 corrected abnormal mitochondrial structures and reduced cellular stress markers. When tested in Drosophila with Barth syndrome, the drug dramatically improved their climbing ability (capacity for physical exertion) and normalized their elevated heart rates-two key symptoms that mirror how the disease affects humans. Furthermore, MA-5 restored normal mitochondrial structure in the Drosophila muscle tissue.
These promising results suggest that MA-5 addresses the largest challenges faced by patients with Barth syndrome, which would significantly improve their quality of life. Phase I clinical trials in Japan have been completed successfully, and the research team is preparing to start Phase II trials soon.
“We’ve validated MA-5 using patient cells, iPS cell models and a Drosophila model of Barth syndrome,” remarks Abe. “The evidence from all of these studies supports its potential effectiveness in patients with Barth syndrome, which we hope to examine more in the next clinical trial.”
Considering the limited options for treatment currently available, this research provides hope for a better future for patients and their families. Critically, MA-5 can be taken orally, which makes administration significantly easier for pediatric patients. It is the first oral medication for Barth syndrome to progress to the clinical trial stage.
The team’s findings suggest that MA-5 could become the first disease-modifying treatment for Barth syndrome, offering new therapeutic options beyond current symptomatic management.
Reference:
Yoshiyasu Tongu, Tomoko Kasahara, Tetsuro Matsuhashi, Yoshitsugu Oikawa, Ryota Akimoto, Yuhan Luo, Sayaka Sekine, Momoka Suzuki, Hitomi Kashiwagi, Shinichiro Kanno, Mitochondria-Homing Drug Mitochonic Acid 5 Improves Barth Syndrome Myopathy in a Human-Induced Pluripotent Stem Cell Model and Barth Syndrome Drosophila Model, The FASEB Journal, https://doi.org/10.1096/fj.202401856RRR.
Powered by WPeMatico

UK: A 14-year observational study published in BMJ Open has revealed a strong link between blood sugar control and the risk of developing several eye diseases in older adults. The research, conducted by Caitlin Lin and Stephen Jivraj from the UCL Global Business School for Health, examined how diabetes status and blood sugar levels influence the likelihood of being diagnosed with glaucoma, diabetic eye disease, macular degeneration, and cataracts over time.
Using data from the English Longitudinal Study of Ageing (ELSA), the study followed over 5,600 participants aged 50 and above across eight waves of data collection from 2004 to 2019. Researchers analyzed nearly 29,000 observations, using logistic regression models to assess the relationship between baseline blood sugar status and the later development of eye conditions.
Participants were grouped based on their diabetic status and glycated hemoglobin (HbA1c) levels: non-diabetic (HbA1c <6.5%, no diabetes diagnosis), controlled diabetes (diagnosed with diabetes, HbA1c <6.5%), uncontrolled diabetes (diagnosed, HbA1c ≥6.5%), and undiagnosed diabetes (no diagnosis, HbA1c ≥6.5%). Adjustments were made for various factors, including age, gender, physical activity, BMI, and smoking.
The study led to the following findings:
According to the researchers, “Our findings suggest that maintaining good blood sugar control in older age not only helps in diabetes management but may also play a crucial role in preventing vision-related complications.”
The study is notable for its use of a large, nationally representative cohort with detailed biomarker and lifestyle data, offering valuable insights into the long-term effects of metabolic health on eye disease. However, the authors acknowledged limitations, such as reduced sample size over time due to participant attrition and the use of subjective physical activity data without duration metrics.
Overall, the study supports routine screening for eye diseases in older adults, particularly those with diabetes or elevated blood sugar levels. It also reinforces the need for early detection and proper glycemic control to help reduce the burden of preventable vision loss in aging populations.
Reference:
Lin C, Jivraj SAre diabetes and blood sugar control associated with the diagnosis of eye diseases? An English prospective observational study of glaucoma, diabetic eye disease, macular degeneration and cataract diagnosis trajectories in older ageBMJ Open 2025;15:e091816. doi: 10.1136/bmjopen-2024-091816
Powered by WPeMatico
