An Instagram post claims that onion juice with sugar dissolves stones in 10-15 days. The claim is FALSE.
Claim
In an Instagram post it is claimed that onion juice with sugar dissolves stones in 10-15 days. In the reel by health.guru008 it is said, “Everyone should know that drinking a syrup made by mixing sugar in onion juice daily for 10 to 15 days can help dissolve and pass stones.”
The claim can be accessed here.
Fact Check
The claim by the user is FALSE. The post fails to clarify which type of stones the remedy targets. While onion may offer certain protective benefits due to its antioxidant properties, the high sugar content in the drink as mentioned can potentially increase the risk of kidney stones. Moreover, gallstones cannot be eliminated through home remedies and typically require surgical removal for effective treatment.
The most common types of stones found in the body are kidney and gall stones.
What are Kidney stones?
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), kidney stones also known as renal calculi are hard, crystalline structures that form within the kidneys but can occur anywhere along the urinary tract. These stones often lead to intense pain, especially when they move through the urinary system.
What are the Factors Contributing to Kidney Stone Formation?
Several factors can contribute to the formation of kidney stones:
Dehydration: Inadequate fluid intake leads to reduced urine output, resulting in higher concentrations of stone-forming minerals.
Diet: Diets high in animal protein, sodium, and refined sugars are associated with an increased risk of certain types of stones.
Medical Conditions: Disorders such as hyperparathyroidism, recurrent urinary tract infections, and various metabolic abnormalities can promote stone development.
Genetic Predisposition: A family history of kidney stones significantly raises an individual’s risk.
Medications: Certain drugs, including diuretics and calcium-containing antacids, may increase the likelihood of stone formation.
What are the treatment strategies for kidney stones?
Kidney stones can be of different sizes. Drinking plenty of fluids can help small stones pass on their own and also dilute the urine, lowering the chances of new stone formation. In contrast, larger stones usually need medical treatment, which may involve surgical or non-surgical options. A variety of treatment options are available for kidney stones, aimed at relieving pain and preventing complications. Shock Wave Lithotripsy (SWL) uses high-energy sound waves to break stones into smaller fragments, allowing them to pass more easily through the urinary tract. Cystoscopy and Ureteroscopy involve inserting a thin scope through the urethra to locate and either extract or fragment stones in the urethra, bladder, or upper urinary tract. For larger or more complex stones, Percutaneous Nephrolithotomy (PCNL) is often advised. This procedure involves making a small incision in the back to insert a nephroscope into the kidney, enabling direct removal of the stone, often with laser-assisted fragmentation. These minimally invasive techniques are selected based on stone size, location, and patient condition, promoting faster recovery and improved outcomes.
What are Gallstones?
Gallstones, medically termed cholelithiasis, are hardened substances that develop in the gallbladder or bile ducts due to imbalances in the composition of bile—a digestive fluid made by the liver. As noted by the National Institute of Diabetes and Digestive and Kidney Diseases, these stones can range in size from minute particles to larger clusters and may lead to pain or other complications if left untreated.
Gallstones are typically classified into two primary types. The more prevalent type, cholesterol gallstones, result from excessive cholesterol in bile, which leads to crystallization. Pigment gallstones, made mainly of bilirubin, a substance formed from the breakdown of red blood cells are more commonly seen in people with liver diseases or blood disorders that raise bilirubin levels.
How are Gallstones Managed?
Treatment options for gallstones depend on factors like symptom severity, stone size, and location, and include both surgical and non-surgical methods. A key aspect of effective treatment often involves gallbladder removal.
Cholecystectomy, or surgical removal of the gallbladder, is widely performed in two forms: laparoscopic, a less invasive option, and open surgery, typically used when there is significant inflammation or infection.
For stones in the bile duct, Endoscopic Retrograde Cholangiopancreatography (ERCP) is a non-surgical method that allows stone removal without removing the gallbladder.
In select cases, shock wave lithotripsy may be used to break the stones into smaller pieces, sometimes paired with ursodiol, a bile acid that helps dissolve cholesterol-rich stones.
What are the Health Benefits Of Onions?
Onions are a low-calorie, nutrient-rich food that enhances flavor without adding fat or cholesterol. A single serving (about 45 calories) provides dietary fiber, vitamin C, vitamin B6, potassium, folate, calcium, and iron. They also contain organosulfur compounds known for their potential role in lowering blood pressure and cholesterol. Notably, onions are a source of quercetin, a flavonoid with anti-inflammatory effects that may inhibit LDL oxidation, support heart health, and help regenerate vitamin E.
Can onion juice with sugar dissolve stones in 10-15 days?
There is no scientific evidence or medical consensus supporting the claim that onion juice mixed with sugar can dissolve or aid in passing kidney stones. Although onions may have some health benefits, it is not a proven remedy. High sugar intake is known to increase the risk of developing kidney stones. Further, gall stones cannot be removed without surgical interventions. Hence, the claim is FALSE.
Onions are rich in bioactive compounds that offer various health benefits. A study published in the International Journal of Molecular Sciences reported that onions are rich in quercetin, a flavonoid known for its strong anti-inflammatory effects.
Additionally, a study published in the Journal of Ethnopharmacology highlighted the antibacterial properties of onions, demonstrating their potential to combat a range of bacterial infections due to their bioactive compounds.
An animal studies suggest that onion extract may offer protective effects against kidney stone formation. In a study by Wahid et al., onion extract has some protective effects against kidney stone formation in rats. The extract improved renal function by mitigating oxidative stress, inflammation, and cellular injury in kidney tissues, highlighting its potential nephroprotective properties.
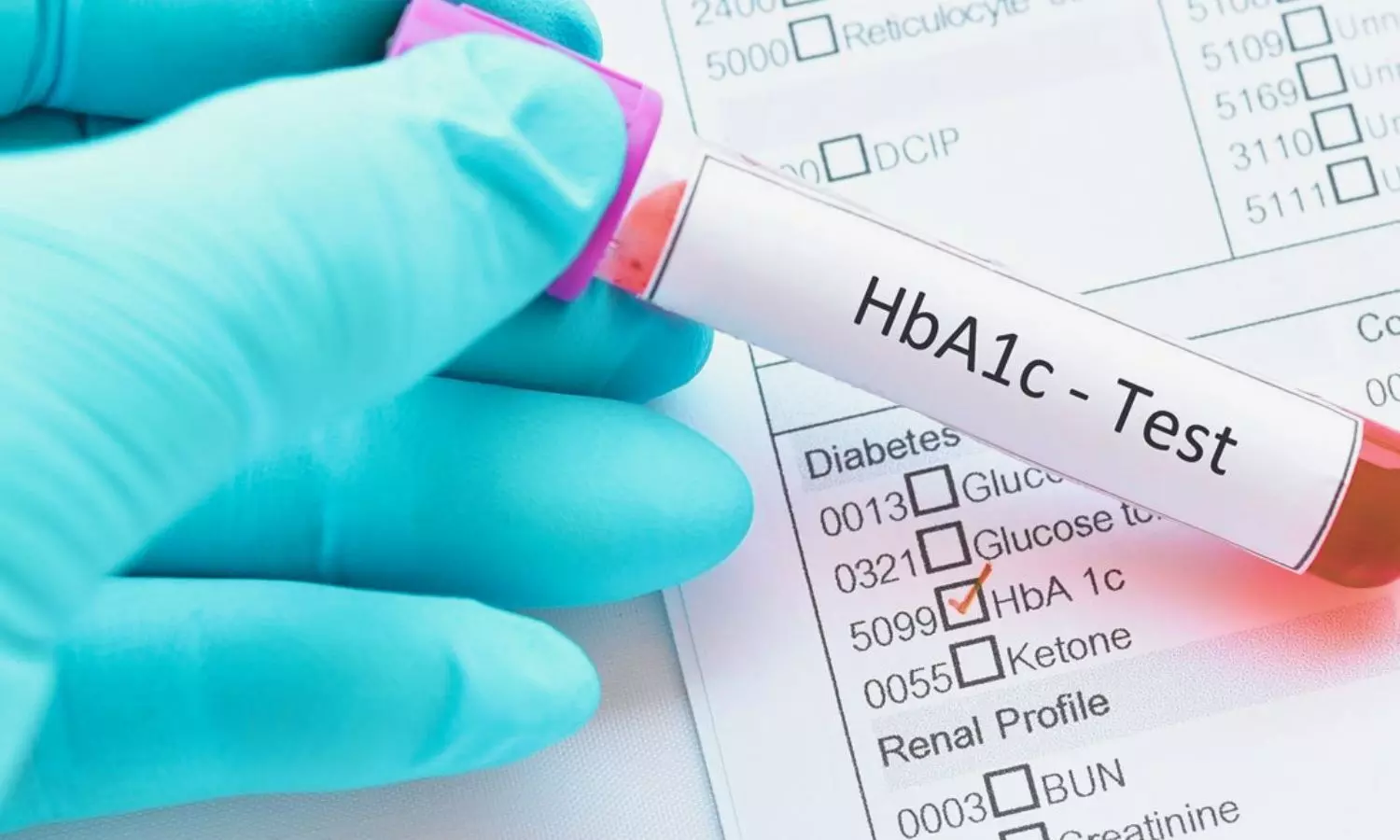
Emerging evidence suggests that high sugar consumption may elevate the risk of kidney stone formation. A study published in Frontiers in Nutrition found that a higher percentage of daily energy intake from added sugars is significantly linked to an increased prevalence of kidney stones.
Similarly, research by Pietro Manuel Ferraro et al. established a correlation between the intake of sugar-sweetened beverages such as soda, punch and a greater likelihood of developing kidney stones.
While onion juice has potential health benefits, strong evidence links high sugar intake to kidney stone formation and gall stones cannot be removed without surgical interventions. Hence, the claim is FALSE.
Talking to The Medical Dialogues Fact Check Team Dr Karunakar Reddy, Senior Gastroenterologist, CARE Hospitals, Hi-tech city, Hyderabad said, “No, drinking onion juice with sugar won’t dissolve kidney stones in 10–15 days. There’s no medical proof that this works. Some small stones may pass on their own if you drink plenty of water, but larger ones usually need proper treatment or procedures. It’s best not to rely on home remedies and instead consult a doctor to avoid complications. No, onion juice with sugar can’t dissolve gallstones either. Gallstones don’t go away that easily. In most cases, if you have symptoms, the best and safest treatment is to remove the gallbladder. Delaying treatment with home remedies might make things worse. Please speak to a specialist and get the right advice.
Dr B Aravind, Senior Nephrologist, CARE Hospitals, Hi-tech city, Hyderabad, further said, “There’s no strong evidence that onion juice with sugar can actually dissolve kidney stones in just 10 to 15 days. Kidney stones come in different sizes and types, so how they’re treated really depends on that. Some home remedies might give some relief, but they won’t replace proper medical care. If you think you have kidney stones, it’s best to check with a doctor who can guide you with the right tests and treatment.
Getting the right treatment early on is important to avoid any complications and help you heal better.”
Medical Dialogues Final Take
The claim that onion juice mixed with sugar can dissolve or pass kidney stones is FALSE. While onions offer certain health benefits, combining them with sugar could be counterproductive, as high sugar intake may actually raise the risk of kidney stone formation. Further gall stones can only be removed by surgical interventions. Moreover, the claim by the user is unsupported by any scientific evidence or medical consensus.
Hence, the claim is FALSE.