High intensity Walking Exercise Program Enhances Stroke Recovery, suggests study
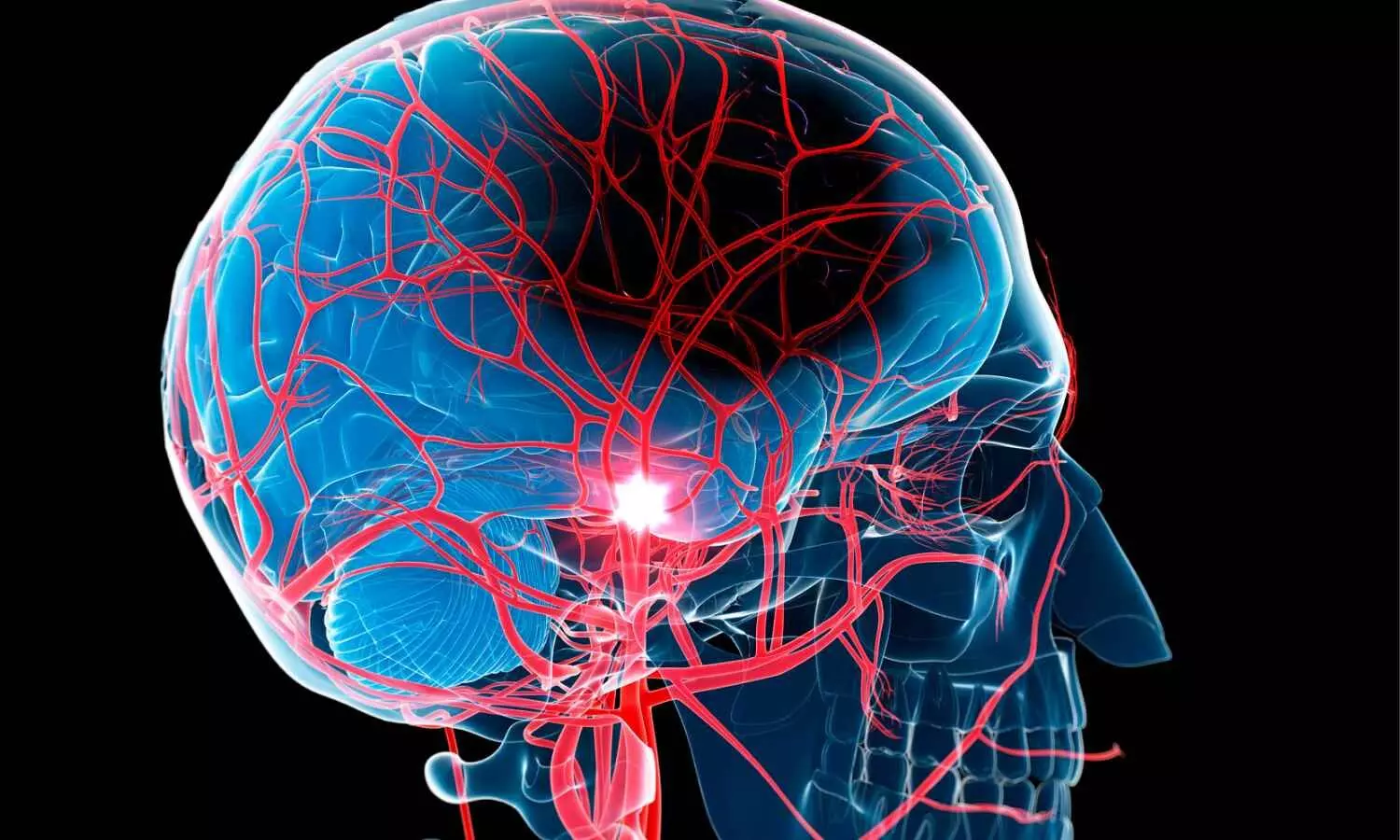
A progressively higher-intensity walking exercise program, combined with standard physical therapy, significantly improved the quality of life and mobility in stroke survivors, according to a preliminary study to be presented at the American Stroke Association’s International Stroke Conference 2025.
Regaining walking ability is an important part of stroke recovery. The 2016 American Stroke Association Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Health Care Professionals recommends that stroke survivors who can participate in three hours of therapy five days a week and who are medically stable should receive care from an inpatient rehabilitation facility.
“Although guidelines recommend structured, progressive exercise after stroke, the uptake of these approaches that have sufficient intensity for rehab programs is still lagging,” said study coauthor Janice Eng, Ph.D., a stroke rehabilitation specialist and a professor in the department of physical therapy at the University of British Columbia in Canada. “Structured and progressively more challenging exercise, aided by wearable devices to provide feedback on intensity, can help people maintain safe intensity levels that are crucial for neuroplasticity — which is the brain’s ability to heal and adapt. The first couple of months after a stroke are when the brain has the greatest ability to change. Our study shows positive results during the initial rehabilitation stage.”
In the study conducted at 12 stroke units across Canada, 306 people were admitted to stroke rehabilitation on average of one month of experiencing anischemic (clot-caused) or hemorrhagic (bleeding) stroke. They were asked to walk for six minutes. At this point, people could walk an average of 152 meters (498 feet — almost the distance of two average city blocks).
Researchers then conducted a blinded trial in which participants were randomized to standard-of-care physical therapy or a new protocol. Based on the participants’ starting point, the protocol objective is a minimum of 30 minutes of daily weight-bearing and walking activities that increase in intensity over time. Participants wore an activity-tracking watch that measured heart rate and number of steps while they walked, which gauged intensity. The new protocol goal was to achieve 2,000 steps with the heart exercising at a moderate intensity for 30 minutes during physical therapy sessions five days a week.
All clinical sites started in the control phase, with 162 participants receiving usual care only and 144 receiving the progressively higher intensity walking intervention. Physical and cognitive abilities, and quality of life were measured at the start of the study and at discharge, about four weeks later. The analysis was adjusted for age, sex and the baseline six-minute walk test time.
The analysis found:
- The improvement on the six-minute walk test was about 43.6 meters (143 feet) greater in the progressively higher intensity walking group compared to the usual care group.
- The progressively higher intensity walking group significantly improved quality-of-life measures, balance and mobility and gait speed.
“The major advance for this study was that we trained all front-line therapists in the stroke units at the 12 sites. The therapists completed the safety screening and ensured the participant’s eligibility for this protocol. We wanted to see what would happen if we moved this protocol into standard-of-care practice so all therapists and all participants could follow this protocol. This was a very successful, real-world trial,” Eng said.
“It is very difficult to change practice. The researchers show that it can be done on the inpatient rehabilitation unit, at a critical period after stroke when the brain is most plastic. The protocol increased endurance and further reduced disability after stroke. This is very positive data for stroke recovery,” said Preeti Raghavan, M.D., chair of the American Stroke Association Rehab and Recovery committee and associate professor of physical medicine and rehabilitation in the Johns Hopkins Department of Physical Medicine and Rehabilitation. Raghavan was not involved in this study.
The limitation of the study is that participants had to be able to take five steps, although assistance from one person was allowed. In some cases, people were not included in the trial because they could not walk, even with assistance.
Study details, background or design:
- There were 306 participants (average age 68; 188 men, 118 women), averaging 29 days since their stroke.
- Researchers used a new study design called a Step Wedge trial, a randomized, blinded study conducted at 12 stroke units across Canada between 2020 and 2022.
- Physical therapists implemented the progressively higher-intensity walking protocol over the first four weeks of the participants’ inpatient rehabilitation stay, when the participants had, on average, been in the hospital for one month since their stroke. The six-minute walk test was measured at the start of the trial and four weeks later to determine its effectiveness.
- All therapists at each stroke unit delivered this protocol to their patients as part of an improved standard of care. The unit was responsible for onboarding new therapists and keeping the protocol in operation.
Reference:
Changing therapy practice to add higher-intensity walking improves early stroke recovery, American Heart Association, Meeting: ASA International Stroke Conference 2025
Powered by WPeMatico