Trump administration puts freeze on release of health info from government agencies
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

New Delhi: A planned two-night
getaway to Kainchi Dham near Nainital turned into a nightmare for the Chairman
of Elantis Healthcare and his daughter after they were duped of Rs 26500 on
the pretext of booking a hotel. The doctor shockingly discovered that the hotel
they booked did not exist.
Dr Mannan Gupta had
booked a hotel called Kainchi Dham Ashram through an online search,
hoping to start the year afresh with a serene trip in early February, reports the Daily. According
to Gupta, a hotel employee claimed the property was inside the Neem
Karoli temple compound, making it seem like an ideal choice. “We wanted to stay
somewhere close to the (Neem Karoli Baba) Ashram (also known as Kainchi Dham),”
said Dr Gupta.
According to The Indian Express, the staff shared the hotel’s bank details with the unsuspecting
doctor. He stated, “The rooms looked simple and the price was nominal… I wanted
to book two rooms.” The doctor had some suspicion as the Bank details did not
have the hotel’s name but the accused assured him that the payment would reach
the hostel for booking.
After the doctor
transferred Rs.13,050 through NEFT, the employee insisted the payment had not
been received. Gupta shared transaction details and screenshots, but the
employee demanded a second payment via UPI, promising to refund the initial
amount. Trusting the assurances, Gupta paid Rs.13,450 through UPI. The Daily reports that the employee then disappeared, leaving Gupta scammed out of Rs.26,500.
The doctor stated, “He
stopped taking my calls, even my accountant’s calls… after calling him
persistently for a day I realised it was a scam. Then I found that no such
hotel existed.” Upon realizing the fraud, Gupta filed a complaint on the
cybercrime portal.
The trend of doctors
falling victim to online fraud is on the rise across the country. In a
similar case, an Indore-based doctor was duped of Rs 3.08 crore by a woman who
lured him with promises of high investment returns.
Powered by WPeMatico

Patna: Bihar Chief Minister Nitish Kumar, on Wednesday, announced plans to construct a new Medical College and Hospital in Araria district. He stated that a team would be formed soon to identify suitable land for the construction of the facility.
During the second phase of his Pragati Yatra, Kumar visited Araria during the day and inaugurated and laid the foundation stones of 449 projects worth Rs 305 crore for the district. He said a Medical College and Hospital would be constructed soon in the district.
According to a UNI report, Kumar said the decision for constructing the Medical College and Hospital was taken to provide better treatment facilities to the people within the district. A team would soon identify land for construction of the Medical College and Hospital.
While reviewing the ongoing schemes in the district, Kumar instructed the authorities concerned to ensure timely action on the issues raised during his Pragati Yatra by various sections of the society.
Also Read:CM Nitish Kumar Inaugurates New Medical College in Chhapra with 100 MBBS seats
He said the cabinet has already taken decisions regarding the demands raised by the people during the ongoing Pragati Yatra.
Highlighting his government’s achievements, Kumar said that it works for everyone without any discrimination and there is complete peace in society.
The Chief Minister said his government made remarkable progress in various sectors including education, health, environment, agriculture, infrastructure, irrigation, Panchayati Raj and others.
Bihar had only six Government Medical College Hospitals when he took over and the number now has increased to 12, Kumar said adding that his government was contemplating further increasing the number of Government Medical College hospitals within the state.
For women empowerment l, special reservation facilities were provided to them following which they were progressing in every walk of life.
During the review meeting the district magistrate of Araria Anil Kumar apprised the chief minister about the progress of various projects and ongoing schemes in the district.
Also Read:Bihar CM lays foundation stone of Mahavir Child Cancer Hospital
Powered by WPeMatico
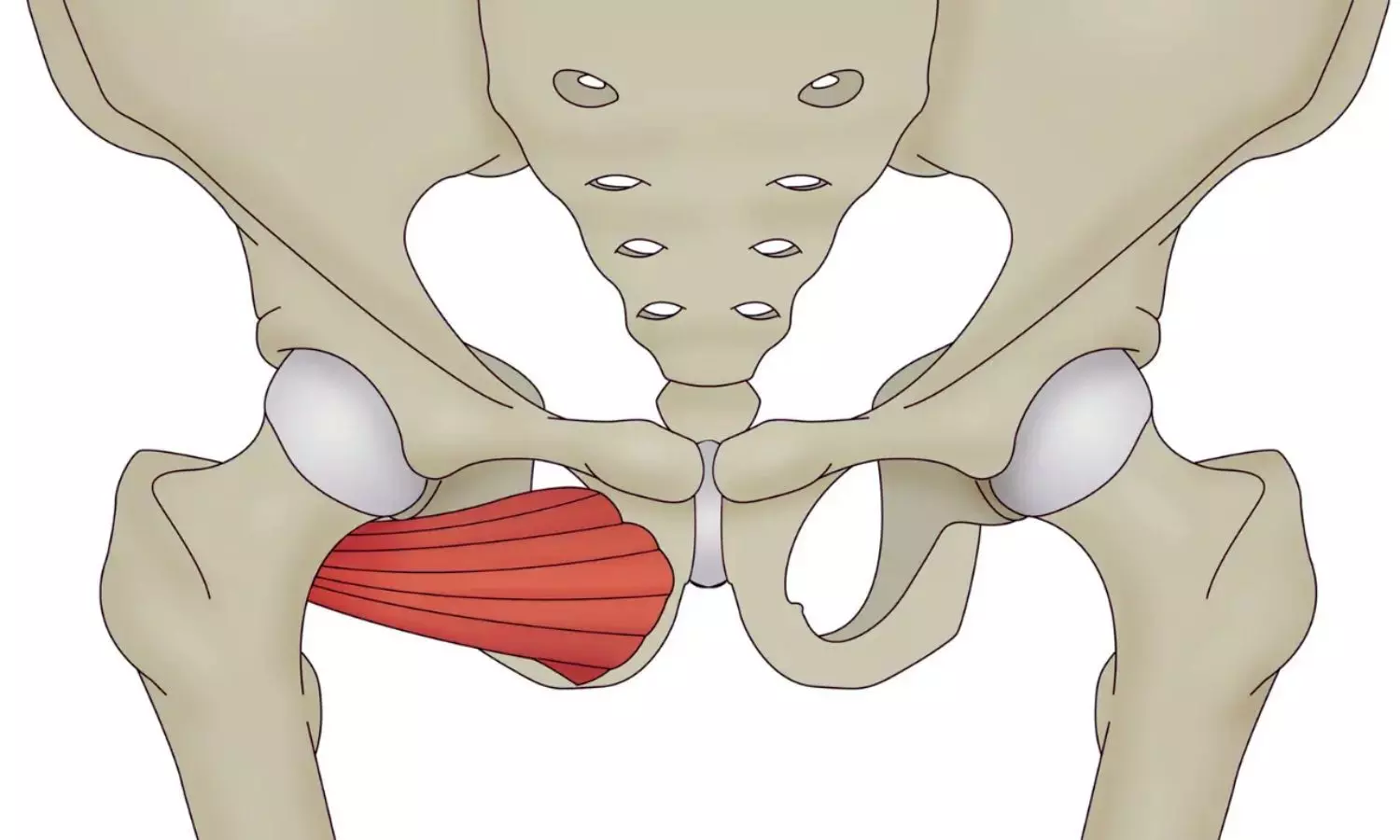
UK: Pelvic stress fractures (PSFs) following pelvic tumor resection and reconstruction are rare but significant complications that can have a profound impact on patient recovery and quality of life. A recent study, published online in Apollo Medicine, highlights the importance of early diagnosis and timely management of this complication. Researchers suggest that radiologists and orthopedic oncology surgeons must be aware of pelvic stress fractures to ensure optimal patient care.
Dr. Rajesh Botchu, the study’s lead author from the Royal Orthopedic Hospital in Birmingham, UK, shared valuable insights with Medical Dialogues. He emphasized that pain following pelvic tumor surgery can stem from several causes, including recurrence of the tumor and implant failures. He added, “Stress response and stress fractures can occur due to altered biomechanics, which can result in pain. These conditions can mimic recurrence on MRI, and awareness of this is essential to decrease morbidity.”
Dr. Botchu further highlighted the clinical implications of the study, stressing that stress fractures can be mistaken for recurrence on MRI. He emphasized that this awareness is crucial in reducing complications and improving patient outcomes.
Pelvic bone tumors are uncommon and can be associated with a poor prognosis, despite advances in radiological imaging and surgical techniques. Limb salvage surgery has become the standard treatment for patients with primary bone sarcomas. However, the rate of peri-operative complications, such as local recurrence and surgical site infections (SSI), remains high.
To explore the occurrence of pelvic stress fractures in this context, Dr. Botchu and his colleagues conducted a retrospective study at their tertiary referral oncology center. The study focused on patients who underwent internal hemipelvectomy for pelvic tumors or sarcomas between 2007 and 2019. Patient demographics, clinical features, imaging results, clinical management outcomes, and peri-operative complications were reviewed.
Out of the patients assessed, six were identified as having developed stress fractures following internal hemipelvectomy. The most commonly affected area was the sacrum, seen in three of the six cases. The ischium and femoral neck were also identified as regions affected by insufficiency stress fractures.
Dr. Botchu acknowledged the limitations of the study and discussed its future directions. “We have shown a case series of stress response and stress fracture-related changes post pelvic surgery. This could probably be replicated in other areas of the body, and further large cohort studies would be helpful to evaluate this further,” he said. When asked about the unique aspects of the study, he mentioned, “This is the first study showing stress response/stress fractures post pelvic surgery.”
“While stress fractures following pelvic resection and reconstruction are rare, they represent a significant complication that warrants attention. The study emphasizes the need for radiologists and orthopedic oncology surgeons to be vigilant and proactive in diagnosing and managing this condition. Early identification of stress fractures can help reduce morbidity and improve patient recovery outcomes,” Dr. Botchu and colleagues concluded.
Reference:
Saad, A., Iyengar, K. P., Kurisunkal, V., Parry, M., & Botchu, R. (2024). Pelvic Stress Fractures Following Resection and Reconstruction of Pelvis Tumours—An Observational Study. Apollo Medicine. https://doi.org/10.1177/09760016241286220
Powered by WPeMatico

A new study published today in the scientific journal Addiction has found that opioid smoking appears to be associated with lower mortality risk compared with opioid injecting. The authors, however, caution that opioid smoking still carries a substantial overdose risk and that these results should not be interpreted as suggesting that opioid smoking is safe.
The study analysed substance use treatment data from 2006 to 2021, comparing 287,481 individuals who reported smoking opioids as their primary form of substance use and an equal weighted number of individuals who reported injecting opioids as their primary form of substance use. The outcome of interest was death during treatment, within one year of treatment admission.
The analysis found a mortality rate of 6.5 per 1000 person-years in the smoking cohort and 9.7 in the injection cohort. The mortality rate ratio was 0.67, meaning people who primarily smoked opioids died at two-thirds of the rate of people who primarily injected opioids.
Although smoking rather than injecting opioids may mitigate some risks, smoking opioids still carries a significant risk of death. Smoking recently surpassed injection as the most common route of administration identified among opioid-related fatal overdoses in the United States, likely driven in part by the rising popularity of opioid smoking and the decrease in opioid injecting.
Lead author Dr. George Karandinos, a clinical and research fellow at Massachusetts General Hospital and Harvard Medical School, comments: “Smoking opioids instead of injecting likely reduces injection-associated complications like the transmission of HIV and hepatitis C and other serious infections. Our study suggests that smoking also appears to be associated with a lower risk of death. Overestimating the safety of smoking, however, could encourage people to lower their vigilance against overdose, eliminating or reversing any potential risk reduction. People who use opioids and those caring for them must understand that while smoking may reduce harm relative to injection, opioid smoking is not safe. People who smoke opioids should still seek treatment, carry naloxone, avoid using opioids while alone, and avoid sharing smoking equipment, which can lead to inadvertent fentanyl resin exposure and overdose.”
Senior author Dr. Daniel Ciccarone adds: “Smoking opioids can be done to deliver a large and rapid dose, as would occur with injection use, and those specific ways of smoking have significant risk for overdose.
Reference:
Dr. George Karandinos, Mortality risk among individuals who smoke opioids compared with those who inject: A propensity score-matched cohort analysis of US national treatment data, Addiction, DOI:10.1111/add.16740.
Powered by WPeMatico
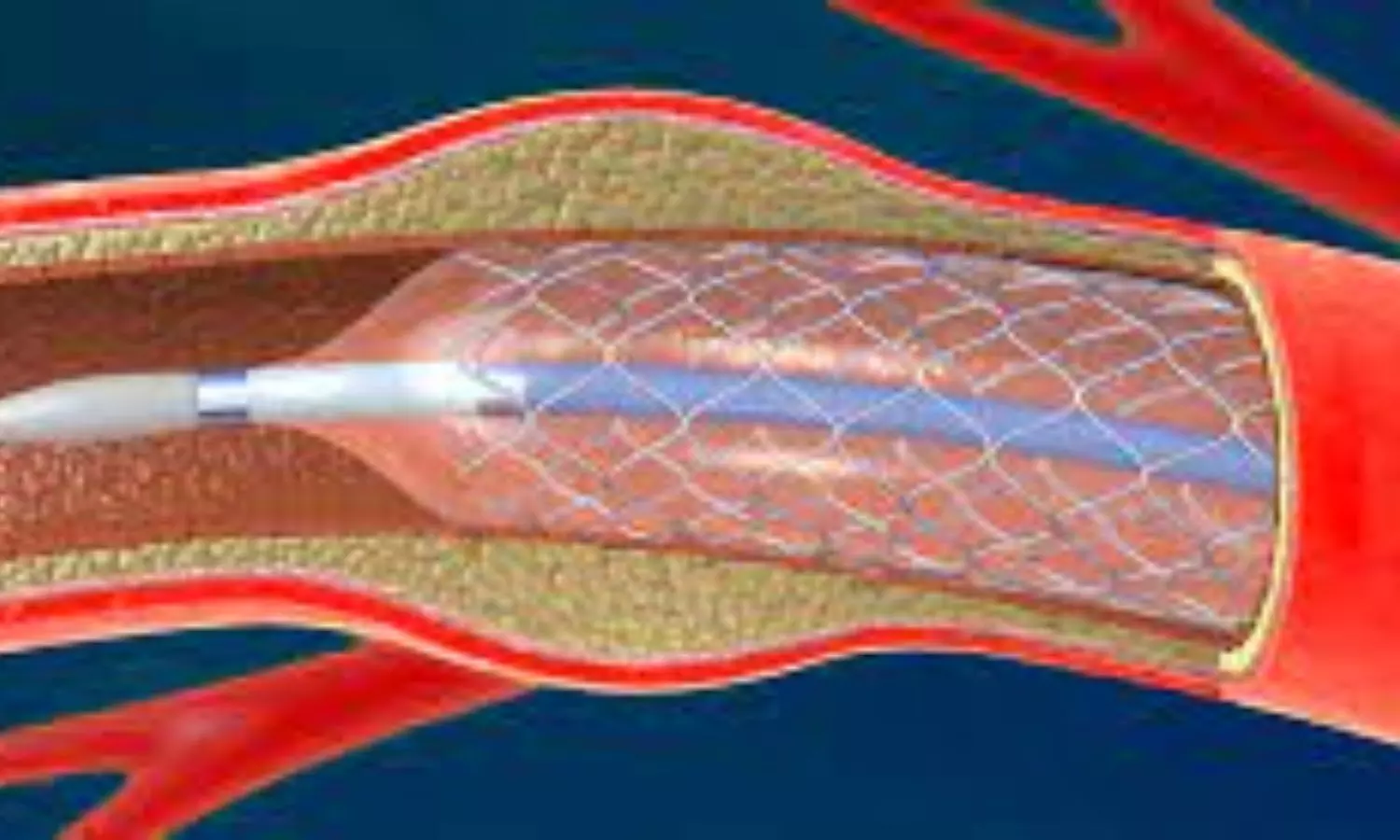
A recent study published in the Stroke; a Journal of Cerebral Circulation found that short-duration dual antiplatelet therapy (DAPT) is as effective and safe as long-duration DAPT for patients undergoing carotid artery stenting (CAS). The findings could help clinicians to optimize post-procedure treatment for patients at risk of complications from extended DAPT use.
Carotid artery stenting (CAS) is a less invasive alternative to carotid endarterectomy for patients with carotid artery stenosis which significantly increases the risk of ischemic stroke. After CAS, DAPT (combination of aspirin and clopidogrel) is prescribed to prevent clot formation and subsequent strokes. This study was set out to determine whether a shorter duration of DAPT could provide comparable protection while minimizing risks of bleeding or other adverse effects.
This research utilized data from the Korean Health Insurance Review and Assessment Service from 2007 to 2019 and analyzed outcomes for 12,034 patients who underwent CAS. This study divided patients into 2 groups based on the duration of DAPT where the patients who received DAPT for at least 90 days but less than six months were included in the Short-DAPT, while the Long-DAPT group comprised patients who maintained DAPT for longer than six months.
The primary outcome assessed was a composite of ischemic stroke, gastrointestinal bleeding, and intracranial hemorrhage within 12 months after transitioning to single antiplatelet therapy. Among the 12,034 patients studied, 2,529 were in the short-DAPT group, while 9,505 were in the long-DAPT group.
In the short-DAPT group, 41 patients (1.6%) experienced ischemic stroke, 22 patients (0.9%) had gastrointestinal bleeding, and 4 patients (0.2%) suffered intracranial hemorrhage. In the long-DAPT group, 108 patients (1.1%) had ischemic stroke, 87 patients (0.9%) experienced gastrointestinal bleeding, and 4 patients (0.04%) suffered intracranial hemorrhage.
The overall rate of the composite primary outcome was similar between the groups (2.5% for short-DAPT versus 2.1% for long-DAPT), with no statistically significant difference (adjusted hazard ratio 0.869; P=0.337). Overall, the study suggests that short-duration DAPT is a viable option after CAS by providing comparable clinical outcomes to long-duration DAPT in terms of stroke prevention and bleeding complications.
Reference:
Yoo, J., Lim, H., & Seo, K.-D. (2025). Optimal duration of dual antiplatelet therapy after carotid artery stenting: A nationwide cohort study. Stroke; a Journal of Cerebral Circulation. https://doi.org/10.1161/strokeaha.124.048743
Powered by WPeMatico
