JAMA study identifies most common long COVID symptoms in children and teens

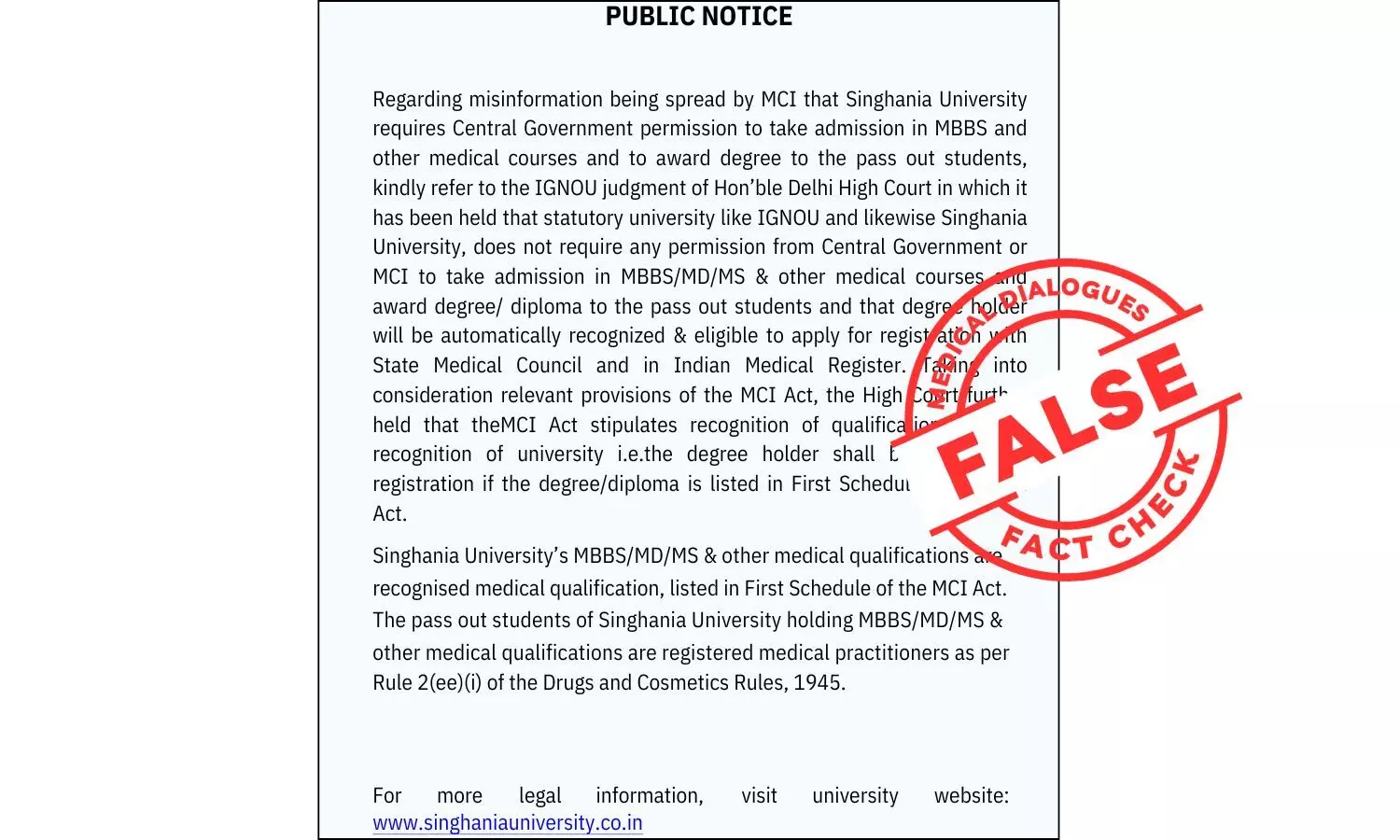
Researchers from the NIH’s RECOVER Initiative have determined what long COVID looks like in youths, based on the most common symptoms reported in a study of over 5,300 school-age children and adolescents.
Using the findings, published in the Journal of the American Medical Association, the researchers also created indices that contain prolonged symptoms-eight for school-age children and 10 for adolescents-that together most likely indicate long COVID.
The indices are not intended to be used in making a clinical diagnosis of long COVID but will guide research to improve diagnosis, treatment, and prevention of the condition in youths.
“Many pediatric and adolescent patients with long COVID have these symptoms, and they are really suffering,” says Melissa Stockwell, Chief of the Division of Child and Adolescent Health and professor of pediatrics at Columbia University’s Vagelos College of Physicians and Surgeons and of population and family health at Columbia’s Mailman School of Public Health, a senior author of the study, and chair of the pediatric coordinating committee for RECOVER. “Knowing which symptoms likely indicate that a child or teen is dealing with long COVID will hopefully help us research how to help patients recover.”
Long COVID in youths
Millions of children in the United States are thought to be living with long COVID-symptoms and conditions that develop, persist, or reoccur weeks or months after a COVID infection.
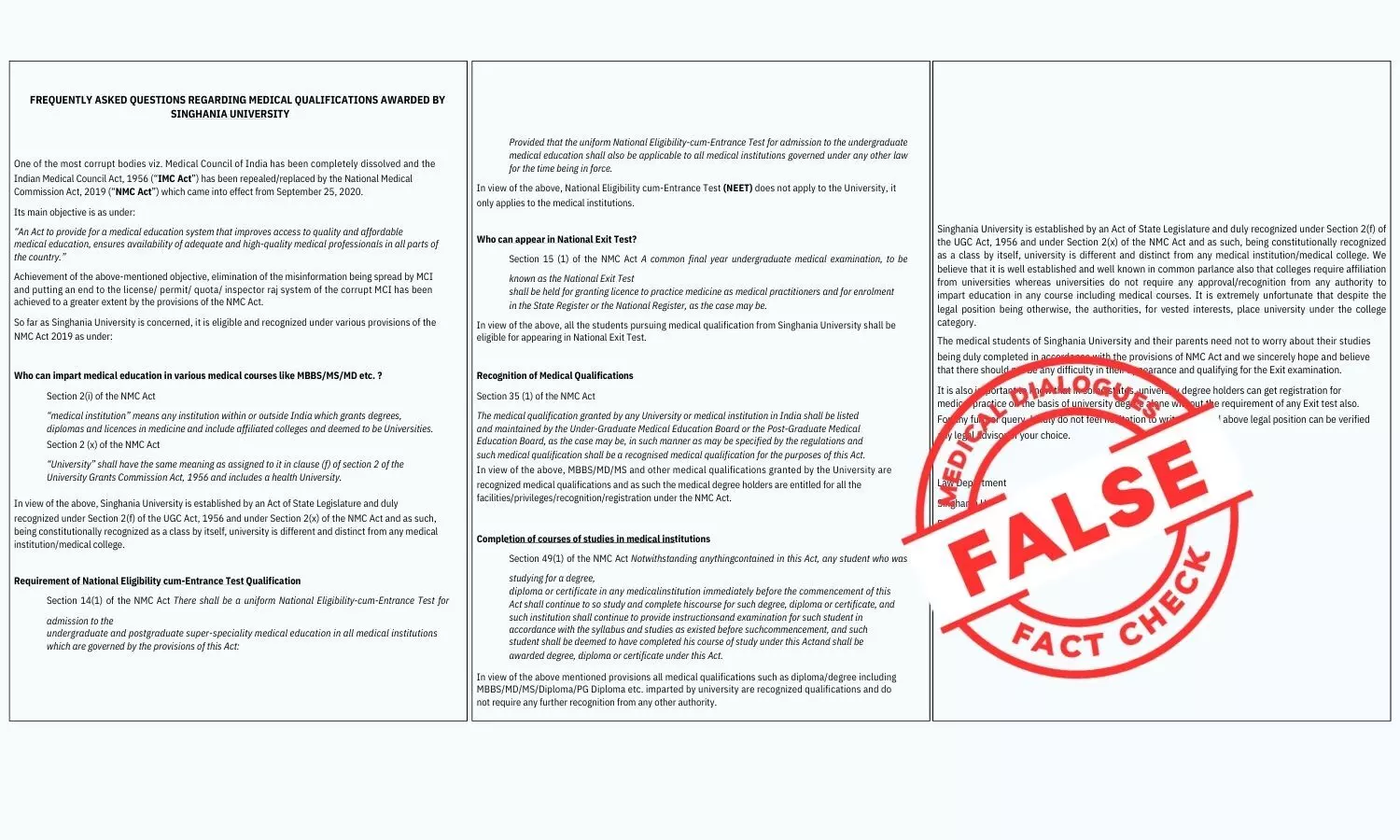
Many health conditions present differently in children than in adults, but the little research on children with long COVID has looked narrowly at one symptom at a time, focusing on symptoms seen in adults with long COVID or lumping all ages together-leading to potential misdiagnoses, delays in diagnosis, or undercounts in the pediatric population.
“This work describes the first data-driven approach to revealing symptom patterns among school-age children and adolescents, which are both distinct from that seen in adults,” says co-first study author Tanayott Thaweethai, PhD, instructor in medicine at Harvard Medical school and lead biostatistician for the RECOVER Initiative.
In the study, the researchers compared prolonged symptoms in children (age 6-11) and teens (age 12-17) with a history of COVID and those with no past infection.
The researchers identified symptoms that were more common in those who were infected. Using statistical analyses, they then identified symptoms that could be combined to form an index that could be used in research studies to determine who likely had long COVID. The indices included 10 symptoms for adolescents and eight for school-age children. Symptoms affected almost every organ system, and most youths had symptoms affecting more than one system.
The researchers uncovered important differences between the two indices. Fatigue, pain, and changes in taste and smell were more prominent in the long COVID index for teens, whereas difficulty focusing, sleep problems, and stomach issues stood out for school-age children.
After the emergence of the Omicron variants in late 2021, the proportion of kids and teens who met the research index threshold for long COVID was lower.
“The research index will likely change and expand as we learn more and is not intended to be used as a clinical tool today,” says corresponding study author Rachel Gross, associate professor in the departments of pediatrics and population health at NYU Langone and co-first author of the study.
“We are proud to be part of this important research to better understand long COVID in the pediatric population,” Stockwell says. “Using the indices as a basis for future research will hopefully help us understand long COVID in children and adolescents, and ultimately develop a robust diagnostic tool to better identify children and adolescents with the condition.”
The researchers are currently using the same approach to develop a research index of long COVID symptoms in younger children.
Powered by WPeMatico