New smartphone-controlled microfluidic device helps with rapid influenza detection
Powered by WPeMatico
Powered by WPeMatico

Karnataka: Shilpa Medicare Limited’s 100 percent subsidiary, Shilpa Pharma Lifesciences Limited’s Active Pharmaceutical Ingredient (API) manufacturing facility, Unit II, situated at Raichur in Karnataka state has received GMP Certification from ANVISA-Brazil.
The GMP inspection was conducted at the facility from April 15-April 19, 2024.
The facility is involved in manufacturing various oncology and nononcology APIs.
“The company remains committed to maintain the GMP status and quality standards as per the expectations and standards of Global Regulatory Authorities,” the Company stated.
Read also: Shilpa Medicare CDMO customer reports positive results from Oxylanthanum Carbonate trial
Shilpa is an integrated pharmaceutical group, headquartered at Raichur, Karnataka, India, with business interests in niche Oncology & Non-oncology APIs, Peptides, Polymers, differentiated finished dosage formulations including orally dispersible films & transdermal patches along with biological portfolio. Shilpa also provides end-to-end CDMO services to global pharmaceutical companies across all its business segments based on its R&D and manufacturing capabilities backed by four R&D units and seven manufacturing facilities.
Read also: USFDA concludes inspection at Shilpa Medicare Hyderabad unit with zero observations
Powered by WPeMatico

Rajasthan- Rajasthan University of Health Sciences (RUHS) has invited applications for admission to BSc Nursing 2024. On this, RUHS has released an information booklet detailing the eligibility, fee, education qualification, and much more.
Below are the details for the admission to B.Sc Nursing, as per the information booklet-
IMPORTANT DATE
|
S.NO |
ACTIVITY |
DATES |
|
1 |
Start date for filling in the online application form at the website. |
25.06.2024 (5.00 pm) |
|
2 |
Last date for depositing the application fees. |
16.07.2024 (11.55 pm) |
|
3 |
The last date for submitting the online application form at the website. |
16.07.2024 (11.55 pm) |
|
4 |
Option to edit incorrect information (if any) entered by the candidate in the online filled application form. |
19.07.2024 to 20.07.2024 (11.55 pm) |
|
5 |
Printing of admit card. |
To be announced later. |
|
6 |
Entrance examination (offline, OMR based). |
To be announced later. |
|
7 |
Printout of the online application form (along with fee payment proof and all relevant documents). |
To be submitted at the time of joining |
APPLICATION FEE
All candidates are required to deposit a non-refundable application fee of Rs. 1800/- (Rs. 900 for SC, ST, ST-STA category of Rajasthan state) using the procedure mentioned in the online application form (plus service charges, as applicable). The application fee is not refundable, not transferable or adjustable for any future RCA Nursing. Any request in this matter shall not be entertained.
ELIGIBILITY CRITERIA FOR ADMISSION
All residents of India fulfilling the eligibility criteria can apply to RUHS for RCA Nursing 2024 for admission to Nursing courses in different government colleges, government self-financed colleges and private colleges affiliated to Rajasthan University of Health Sciences, Jaipur (State Government Medical University), based on instructions given in this information booklet, the relevant rules of RUHS, Jaipur and directions of State Govt. / Honorable Court. For admission to B.Sc Nursing courses in colleges affiliated with RUHS, it is mandatory to appear in the B.Sc Nursing Entrance Examination 2024 [Rajasthan Centralized Admissions to Nursing Courses 2024, (RCA Nursing 2024)].
EDUCATION QUALIFICATION
A candidate must have passed the Senior Secondary School Certificate Examination (ScienceMedical group) conducted by a statutory Board at the end of 12 years of study under the 10+2 pattern of Secondary Education in all the compulsory subjects and the optional subjects of the Medical Group (Physics, Chemistry and Biology and English) or any other examination recognised by the RUHS as equivalent to above-stated qualification on the last date of submission of application form with a minimum of forty-five per cent (45%) marks and forty per cent (40%) for natural born scheduled caste and scheduled tribe candidates in aggregate of Physics, Chemistry and Biology taken together at the qualifying examination and with English as a compulsory subject in class 10+2 for being eligible for admission to B.Sc Nursing course.
AGE LIMIT
A candidate must have completed the age of 17 years but not completed 28 years in the case of females and 25 years in the case of males on or before 31st December 2024. The date of birth as recorded in the secondary education certificate will be treated as authentic.
TENTATIVE SEAT MATRIX (2024-25)
Admission for the session 2024-25 will be considered in the colleges after finalisation of the list of colleges by RUHS. Based on the B.Sc Nursing ordinance, 85% of the total seats will be filled up by the Bonafide candidates of Rajasthan, and 15% of the total seats will be filled up by the candidates on an India basis inclusive of Rajasthan as per State Government guidelines and/or Hon’ble Court directions. The percentage of female candidates shall not fall below 50% of the total seats in all categories. As per the government order dated from the academic session 2023-24, in all the nursing colleges, 100% of seats (of the intake sanctioned) shall be filled through RCA Nursing 2024. College and course-wise tentative seat matrix for the session 2024-25 will be made available at the RUHS website before choice filling.
FEE STRUCTURE
Based on the directions of the State Govt. / State Level Fee Fixation Committee, the fee structure for the B.Sc Nursing course for the session 2024-25 is as below-
|
S.NO |
GOVT. COLLEGES (UNDER SFS) |
GOVT. NURSING COLLEGE JAIPUR |
GOVT. (RAJMES NURSING COLLEGES |
PRIVATE SELF-FINANCED NURSING COLLEGES |
|
1 |
Boys (General, OBC, MBC, EWS) 50,000/- per annum + Caution money as applicable. Boys (SC, ST) and all Girls 20,000/- per annum + Caution money as applicable |
As prescribed by the State Government |
Boys (General, OBC, MBC, EWS) 50,000/- per annum + Caution money as applicable Boys (SC, ST) and all Girls 20,000/- per annum + Caution money as applicable |
95,000/- per annum + Caution money as applicable. |
The candidates are required to pay the fee as prescribed by State Government from time to time, for the course.
CHOICE FILLING
After appearing in the entrance examination, to participate in the counselling process, candidates will be required to fill choices of the course and college (in order of preference) by paying INR 550 (five hundred and fifty) as counselling fee (non-refundable). Guidelines for filling out the choices and making online payment of counselling fees will be available on the RUHS website in due course.
To view the information booklet, click the link below
Powered by WPeMatico

Bhopal: Raising serious concerns about the practice of unqualified MBBS doctors performing caesarean section deliveries in private hospitals across the state, a Public Interest Litigation (PIL) has been filed in the principal bench of the Madhya Pradesh High Court at Jabalpur seeking a high-level probe into the matter.
The PIL, driven by Vijay Bajaj and his advocate Aditya Singh sought a thorough investigation into the regular performance of C-section procedures in private hospitals across the state and also requested an inquiry into the reasons why MBBS doctors, rather than qualified gynecologists, are performing these procedures.
The PIL follows a complaint made to the Harda district collector, which claimed that 100 C-section procedures were performed in a private hospital in Harda by MBBS doctors. The complaint was also forwarded to the Madhya Pradesh Medical Council in Bhopal, which subsequently referred the case to the Chief Medical and Health Officer (CMHO) of Harda.
Also read- BAMS Doctor Performs Delivery At Patiala Nursing Home, Patient Dies Of Postpartum Haemorrhage
As per the latest Free Press Journal news report, Adv Aditya Singh said, “We have cited an example of Harda. This is not a lone case; there are many such hospitals in the state where MBBS doctors are performing C-section procedures which only specialists are authorized to perform. We have demanded a high-level probe into the matter.”
Medical Dialogues team had earlier reported a similar incident where a BAMS (Bachelor of Ayurvedic Medicine and Surgery) doctor allegedly conducted delivery of a 31-year-old patient at a private nursing home in Patiala instead of a gynaecologist following which the patient reportedly died from postpartum haemorrhage.
There are reportedly more cases where MBBS doctors perform instead of gynaecologists, the PIL further sought detailed reports on the number of gynaecologists employed in private hospitals for performing deliveries, whether by C-section or natural birth. It also demanded a comparison of the ratio of C-section procedures performed in private hospitals versus government hospitals in the state.
The PIL highlights that, according to the Ministry of Health and Family Welfare, only in emergencies or when there is no chance of securing a specialized gynaecologist, can a cesarean section be performed by an MBBS doctor or a general surgeon. However, the petition stated when a gynaecologist is available, but for reasons which are difficult to understand but easy to infer, under any circumstances, the caesarean procedure cannot be performed by an MBBS doctor or by a general surgeon.
Powered by WPeMatico

Taiwan: Oral antidiabetic therapy is not inferior to early insulinization for managing glycemic control in newly diagnosed type 2 diabetes patients, regardless of their initial HbA1c levels, a recent study has found.
The findings, published in Scientific Reports, support oral therapy as a rational treatment option, even in those with elevated HbA1c at diagnosis.
Type 2 diabetes mellitus (T2DM) is a chronic condition characterized by insulin resistance and relative insulin deficiency. Effective management of blood glucose levels is crucial to mitigate the risk of complications such as cardiovascular disease, neuropathy, and nephropathy. Traditionally, treatment strategies have included oral antidiabetic medications (OADs) and, in some cases, early initiation of insulin therapy.
Against the above background, Yang-Ming Lee, Department of Internal Medicine, Changhua Christian Hospital, Changhua, Taiwan, and colleagues aimed to compare the efficacy of oral antidiabetic therapy to early insulinization on glycemic control among newly diagnosed T2D patients in real-world clinical practice.
For this purpose, the researchers conducted a retrospective cohort study at a medical center in Taiwan analyzing 1256 eligible patients from 2007 to 20177. Propensity score matching ensured that the oral antidiabetic drug (OAD) and early insulinization cohorts comprised well-balanced groups, each consisting of 94 patients. Glycemic outcomes were subsequently evaluated across both cohorts.
The researchers reported the following findings:
The findings showed that early initiation of insulin may not yield substantial improvements in glycemic control for newly diagnosed type 2 diabetes patients when compared to using OADs alone. Simply starting insulin early is inadequate; achieving optimal control requires implementing a structured insulin titration protocol and diligent self-monitoring of blood glucose levels.
“Our real-world data support considering oral antidiabetic therapy as a reasonable treatment option for newly diagnosed T2D patients, even those with increased baseline HbA1c levels,” the researchers wrote.
“Finally, while this study offers valuable insights from a specific hospital setting, its findings could be influenced by significant limitations. Thus, further investigation is needed to determine the applicability of these findings to other regions in Taiwan or different countries,” they concluded.
Reference:
Lee, Y., Lin, P. R., & Sia, H. (2024). Oral antidiabetic therapy versus early insulinization on glycemic control in newly diagnosed type 2 diabetes patients: A retrospective matched cohort study. Scientific Reports, 14(1), 1-9. https://doi.org/10.1038/s41598-024-66468-1
Powered by WPeMatico
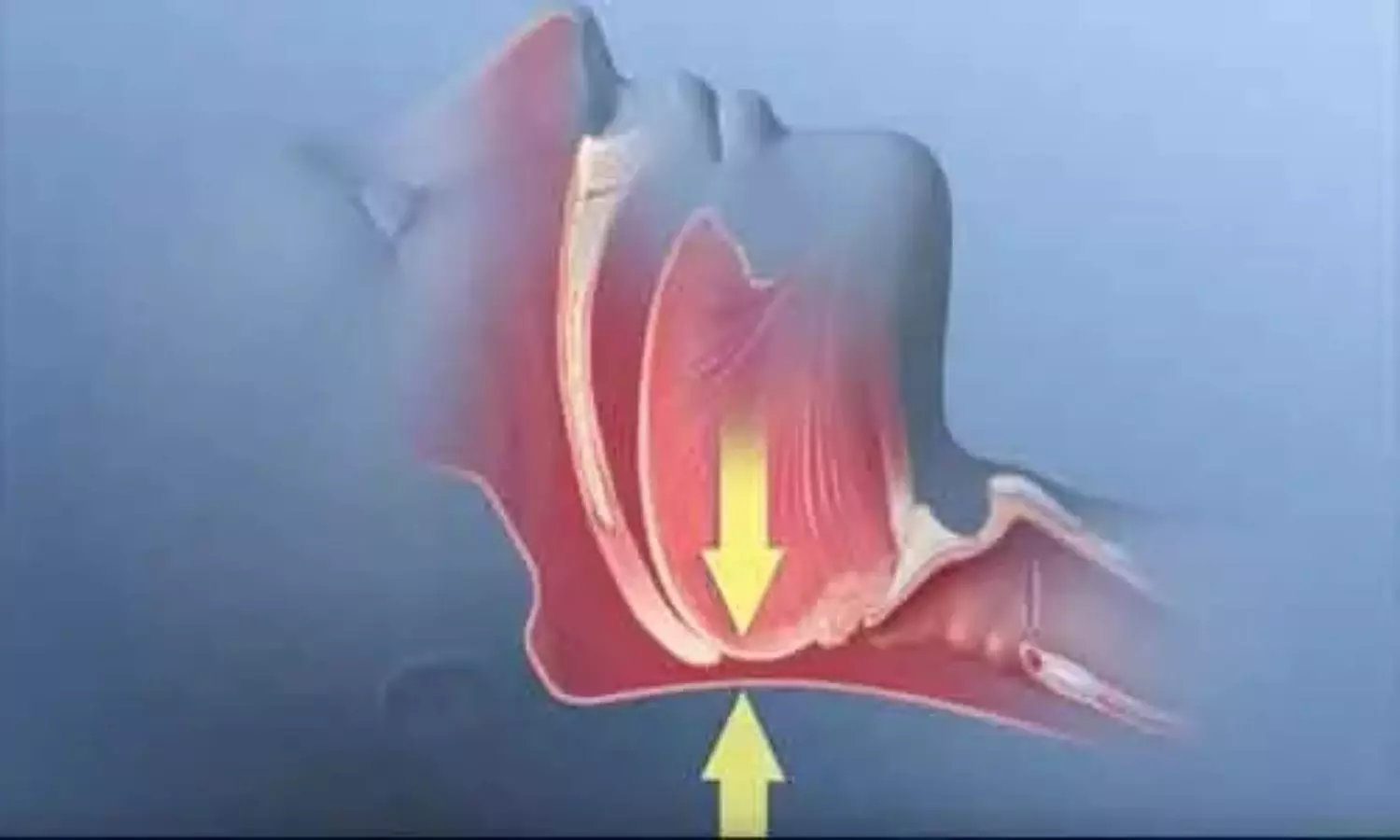
USA: A recent study comparing the effects of metabolic surgery versus usual care on cardiovascular outcomes in patients with obstructive sleep apnea (OSA) and obesity has yielded significant findings, shedding light on potential therapeutic benefits beyond traditional treatments. The study underscores the critical role of surgical interventions in managing complex health conditions like OSA and obesity.
The study, published in the Journal of the American College of Cardiology, showed that metabolic surgery, compared with nonsurgical management, was associated with a significantly lower risk of incident major adverse cardiovascular events (MACE) and death in patients with moderate-to-severe obstructive sleep apnea and obesity.
Obstructive sleep apnea, characterized by interruptions in breathing during sleep due to airway obstruction, is closely linked with obesity. Both conditions independently increase the risk of cardiovascular diseases such as hypertension, coronary artery disease, and stroke. Traditional treatments for OSA include continuous positive airway pressure (CPAP) therapy and lifestyle modifications aimed at weight loss.
No therapy has been shown to reduce the risk of MACE and death in patients with OSA. Considering this, Ali Aminian, Bariatric and Metabolic Institute, Cleveland Clinic, Cleveland, OH, and colleagues aimed to investigate the long-term relationship between metabolic surgery and incident MACE in patients with OSA and obesity.
For this purpose, the researchers identified adult patients with a BMI of 35-70 kg/m2 and moderate-to-severe OSA in a US health system (2004-2018). Patients who underwent metabolic surgery and those in the nonsurgical control group were well-matched in baseline characteristics using overlap weighting methods. Time-to-incident MACE was estimated using multivariable Cox regression analysis, with follow-up concluding in September 2022.
The study led to the following findings:
In conclusion, the study highlights metabolic surgery as a promising intervention for reducing adverse cardiovascular outcomes in patients with obstructive sleep apnea and obesity. As research continues to evolve, these findings advocate for considering surgical options alongside traditional therapies to optimize health outcomes and improve the quality of life for affected individuals.
Reference:
Aminian, A., Wang, L., Al Jabri, A., Wilson, R., Bena, J., Milinovich, A., Jin, J., Heinzinger, C., Pena-Orbea, C., Foldvary-Schaefer, N., Nissen, S. E., & Mehra, R. (2024). Adverse Cardiovascular Outcomes in Patients with Obstructive Sleep Apnea and Obesity: Metabolic Surgery versus Usual Care. Journal of the American College of Cardiology. https://doi.org/10.1016/j.jacc.2024.06.008
Powered by WPeMatico

Italy: A recent analysis from an Italian cohort study revealed that long-term cancer survivors tended to have longer lifespans when adhering to a Mediterranean diet.
After nearly 13 years of follow-up, cancer survivors who adhered closely to the Mediterranean diet experienced a 32% lower risk of all-cause mortality compared to those with low adherence (hazard ratio 0.68), the researchers reported in JACC: CardioOncology.
The findings suggested the benefit of maintaining or adopting a traditional [Mediterranean diet] even after a cancer diagnosis and motivated the additional science concerning the development of dietary recommendations specifically targeted at cancer survivors.
The Mediterranean diet includes foods naturally rich in polyphenols and bioactive compounds known for their antioxidant, anti-inflammatory, and potential antitumor properties. These benefits are relevant to cancer prevention and progression and play a significant role in preventing cardiovascular mortality.
Research investigating the connections between the Mediterranean diet (MD) and mortality in cancer survivors has yielded inconclusive results. The majority of studies originate from the United States, with limited evidence available from Europe. Additionally, many studies focus on specific types of cancer survivors, which restricts the applicability of findings to the broader population of cancer survivors.
Against the above background, Marialaura Bonaccio, Department of Epidemiology and Prevention, IRCCS Neuromed, Pozzilli, Italy, and colleagues aimed to clarify the role of a traditional MD among Italian long-term cancer survivors concerning mortality, using postdiagnosis dietary data.
Using data from the Moli-sani cohort, established in Italy between 2005 and 2010, which included 24,325 adults aged 35 years or older, the study focused on 802 participants diagnosed with cancer at baseline. These individuals provided medical records and details on cancer treatment. Dietary habits were assessed using a semiquantitative food frequency questionnaire administered by interviewers.
The study group comprised 476 women (59%) and 326 men (41%), with an average age of 63 years. Diet assessment occurred approximately 8.8 years after their cancer diagnosis.
Participants’ adherence to the Mediterranean diet was evaluated using a 9-point scale, categorized as poor (scores 0-3), average (scores 4-5), or high (scores 6-9). Those with higher adherence tended to have a higher socioeconomic status and were more likely to engage in regular physical activity compared to those with poor adherence.
The following were the key findings of the study:
“Our results indicate that continuing or adopting a traditional Mediterranean diet following a cancer diagnosis could offer benefits,” the researchers concluded. “This underscores the need for further research to develop tailored dietary guidelines for cancer survivors.”
Reference:
Bonaccio M, et al “Mediterranean diet is associated with lower all-cause and cardiovascular mortality among long-term cancer survivors” JACC CardioOncol 2024; DOI: 10.1016/j.jaccao.2024.05.012.
Powered by WPeMatico

Researchers in a recent study have found the association between vitamin D levels and the risk of thyroid cancer (TC). This study was published in Frontiers in Nutrition which was conducted by Hu Y. and colleagues. The study aimed to consolidate existing evidence to determine if vitamin D deficiency contributes to a higher susceptibility to TC.
A systematic search of multiple databases including PubMed, Embase, Web of Science, Cochrane, and ClinicalTrials.gov identified relevant articles on vitamin D and TC. The meta-analysis assessed vitamin D levels in individuals with TC compared to controls, evaluating standardized mean differences (SMD), ratio of means (RoM), and odds ratios (OR). Dose-response meta-analysis techniques were employed to quantify the correlation between vitamin D levels and TC risk. Subgroup analyses and meta-regressions were conducted to explore potential sources of variation, while publication bias was assessed using Begg’s and Egger’s tests.
The meta-analysis revealed significant associations:
Individuals with thyroid cancer had lower levels of vitamin D compared to controls (SMD = -0.25, 95% CI: -0.38 to -0.12).
Levels of 1,25 (OH)D were also lower in thyroid cancer cases than in controls (SMD = -0.49, 95% CI: -0.80 to -0.19).
Vitamin D deficiency was associated with a 49% increased risk of thyroid cancer (OR = 1.49, 95% CI: 1.23 to 1.80).
Each 10 ng/ml decrease in 25 (OH)D levels was linked with a 6% increase in thyroid cancer risk (OR = 0.94, 95% CI: 0.89 to 0.99) according to dose-response analysis.
Researchers have found evidence linking vitamin D deficiency with an increased risk of thyroid cancer. Individuals diagnosed with thyroid cancer consistently showed lower vitamin D levels compared to controls, highlighting a potential role for vitamin D in modulating thyroid cancer risk. This meta-analysis underscores the importance of maintaining adequate vitamin D levels, suggesting potential implications for public health strategies aimed at reducing thyroid cancer incidence.
Reference:
Hu Y, Xue C, Ren S, Dong L, Gao J and Li X. Association between vitamin D status and thyroid cancer: a metaanalysis. Front. Nutr. 2024.
Powered by WPeMatico
Women in Europe are receiving more cycles of in vitro fertilisation (IVF) and intrauterine insemination (IUI), according to data presented today at the ESHRE 40th Annual Meeting in Amsterdam.
Preliminary data from the ESHRE European IVF Monitoring (EIM) Consortium [2] reveals a steady and progressive rise in the use of Assisted Reproductive Technology (ART). In 2021, a total of 1 103,633 ART treatment cycles were reported by 1,382 clinics across 37 European countries – a 20% increase from the 919,364 cycles reported in 2020, keeping in mind that this was the year COVID affected the number of treatment cycles [3].
Of these 2021 treatment cycles, 153,191 were IVF, 418,069 intracytoplasmic sperm injection (ICSI), 368,464 frozen embryo replacement, 78,432 preimplantation genetic testing, 79,510 egg donations, 415 in vitro maturation of oocytes, and 5,552 cycles with frozen oocyte replacement. In addition, data from 1,441 institutions reported 148,194 IUI treatments where the partner’s semen is used (31 countries) and 48,583 IUI treatments where donor semen is used (23 countries). A total of 28,768 fertility preservation interventions, including oocyte, ovarian tissue, semen, and testicular tissue banking, were reported from 15 countries.
Clinical pregnancy rates [4] per aspiration and per transfer remained similar in 2021 and 2020 for IVF (26.3% and 33.5 % in 2021 versus 25.4% and 33.2% in 2020) and for ICSI (23.9% and 33.5% in 2021 versus 25.2% and 33.0% 2020). Pregnancy rates per transfer for frozen embryo replacement with own embryos was slightly higher in 2021 (37.0%) versus 2020 (36.0%), as were pregnancy rates per fresh embryo transfer from egg donations (53.1% in 2021 versus 51.3% in 2020), while for frozen oocyte replacements the number decreased slightly (45.5% in 2021 versus 45.7% in 2020).
This reflects a 3.98% increase in the use of one embryo per transfer, rising from 57.9% in 2020 to 60.5% in 2021. The proportion of singleton, twin, and triplet deliveries was 90.4%, 9.5%, and 0.1% in 2021, respectively, compared to 88.9%, 10.9%, and 0.2% in 2020. Twin and triplet delivery rates after frozen embryo replacement were 6.9% and 0.1%, respectively, compared to 7.9% and 0.1% in 2020.
The lead author, Dr. Jesper Smeenk of Elisabeth-TweeSteden Hospital in Tilburg, Netherlands, stated: “The 25th ESHRE report on ART and IUI shows a continuous increase of reported treatment numbers and medically assisted reproduction (MAR)-derived live births in Europe. Being already the largest data collection on MAR in Europe, continuous efforts to stimulate data collection and reporting strive for future quality control and completeness of the data and offer higher transparency and vigilance in the field of reproductive medicine.”
Professor Dr. Karen Sermon, Chair of ESHRE, added: “This report underscores the significance of collaborative efforts and standardized reporting in advancing reproductive medicine. By enhancing data collection practices, we aim to elevate clinical standards and patient outcomes across Europe.”
Reference:
IVF and IUI treatment cycles increase across Europe, along with stable pregnancy rates, European Society of Human Reproduction and Embryology, Meeting:ESHRE 40th Annual Meeting.
Powered by WPeMatico

Stephan Klessinger et al conducted a Systematic review of the literature and subsequent meta-analysis for the development of a new guideline. It has been published in ‘Global Spine Journal’.
This manuscript summarizes the recommendations from a new clinical guideline published by the German Spine Society. It covers the current evidence on recommendations regarding the indication, test blocks and use of radiofrequency denervation. The guidelines aim is to improve patient care and efficiency of the procedure.
A multidisciplinary working group formulated recommendations based on the Grades of Recommendations, Assessment, Development, and Evaluation (GRADE) approach and the Appraisal of Guidelines for Research and Evaluation II (AGREE II) instrument.
20 clinical questions were defined for guideline development, with 87.5% consensus achieved by committee members for one recommendation and 100% consensus for all other topics. Specific questions that were addressed included clinical history, examination and imaging, conservative treatment before injections, diagnostic blocks, the injected medications, the cutoff value in pain-reduction for a diagnostic block as well as the number of blocks, image guidance, the cannula trajectories, the lesion size, stimulation, repeat radiofrequency denervation, sedation, cessation or continuation of anticoagulants, the influence of metal hardware, and ways to mitigate complications.
The authors concluded – “Clinical trials evaluating RF denervation are characterized by widely disparate outcomes, and there is enormous variation in selecting patients and performing procedures. A multidisciplinary working group developed a national clinical guideline for RF denervation of the spine and the SI joint in adult patients. These multi-society guidelines have been developed to improve outcomes, enhance safety, and minimize unnecessary tests and procedures. The recommendations are based on limited evidence or on consensus but are well aligned with recommendations from similar international guidelines. The guideline working groups strongly recommend that research efforts in relation to all aspects of the management of LBP and RF denervation be intensified.”
Further reading:
Radiofrequency Denervation of the Spine and the Sacroiliac Joint: A Systematic Review based on the Grades of Recommendations, Assesment, Development, and Evaluation Approach Resulting in a German National Guideline
Stephan Klessinger et al
Global Spine Journal 2024
DOI: 10.1177/21925682241230922
Powered by WPeMatico
