As part of the University of Colorado Department of Medicine’s annual Research Day, held on April 23, faculty member Christine Swanson, MD, MCR, described her National Institutes of Health-funded clinical research on whether adequate sleep can help prevent osteoporosis.
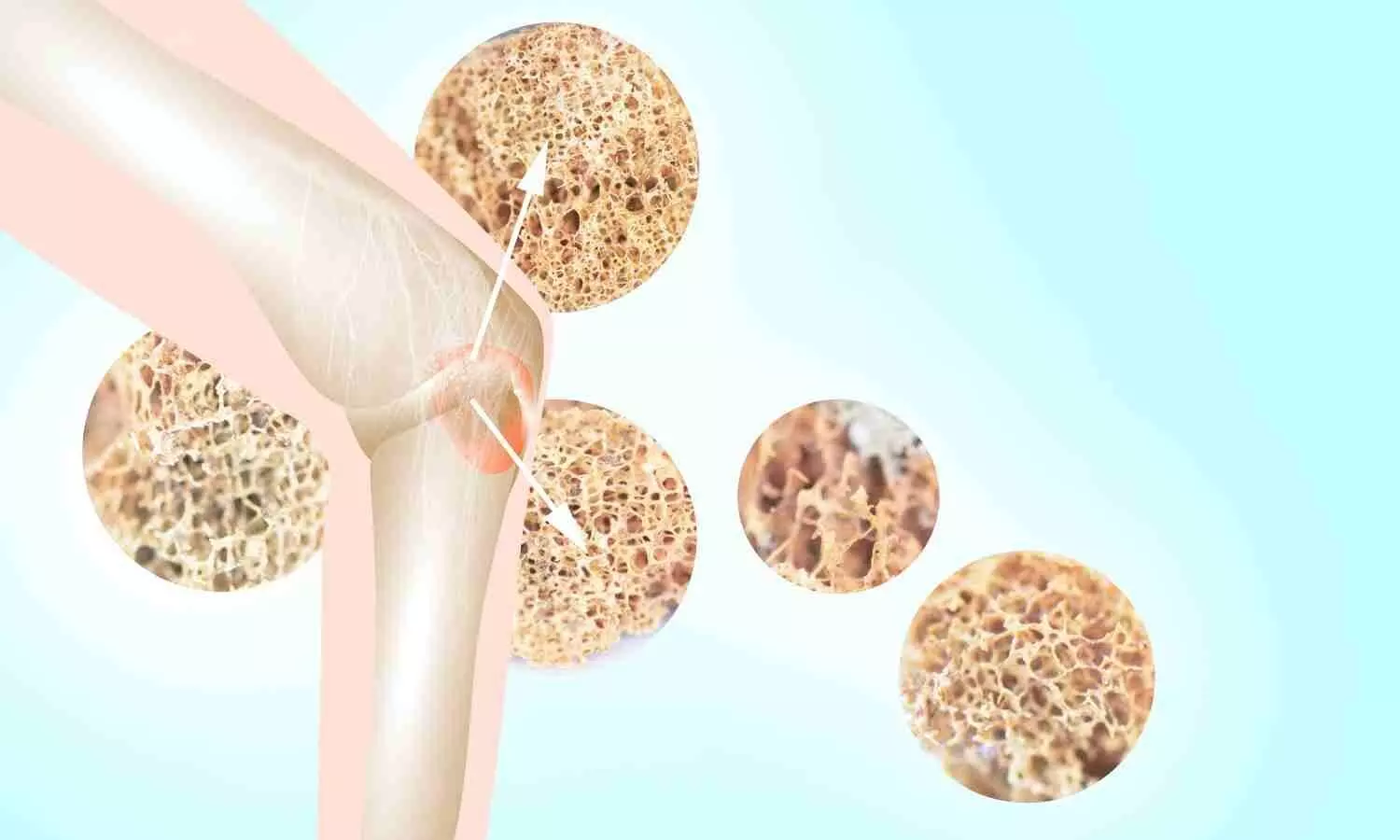
“Osteoporosis can occur for many reasons such as hormonal changes, aging, and lifestyle factors,” said Swanson, an associate professor in the Division of Endocrinology, Metabolism, and Diabetes. “But some patients I see don’t have an explanation for their osteoporosis.
“Therefore, it’s important to look for novel risk factors and consider what else changes across the lifespan like bone does-sleep is one of those,” she added.
How bone density and sleep change over time
In people’s early- to mid-20s, they reach what is called peak bone mineral density, which is higher for men than it is for women, Swanson said. This peak is one of the main determinants of fracture risk later in life.
After reaching this peak, a person’s bone density remains roughly stable for a couple of decades. Then, when women enter the menopausal transition, they experience accelerated bone loss. Men also experience bone density decline as they age.
Sleep patterns also evolve over time. As people get older, their total sleep time decreases, and their sleep composition changes. For instance, sleep latency, which is the time it takes to fall asleep, increases with age. On the other hand, slow wave sleep, which is deep restorative sleep, decreases as we age.
“And it’s not just sleep duration and composition that change. Circadian phase preference also changes across the lifespan in both men and women,” Swanson said, referring to people’s preference for when they go to sleep and when they wake up.
How can sleep relate to our bone health?
Genes that control our internal clock are present in all of our bone cells, Swanson said.
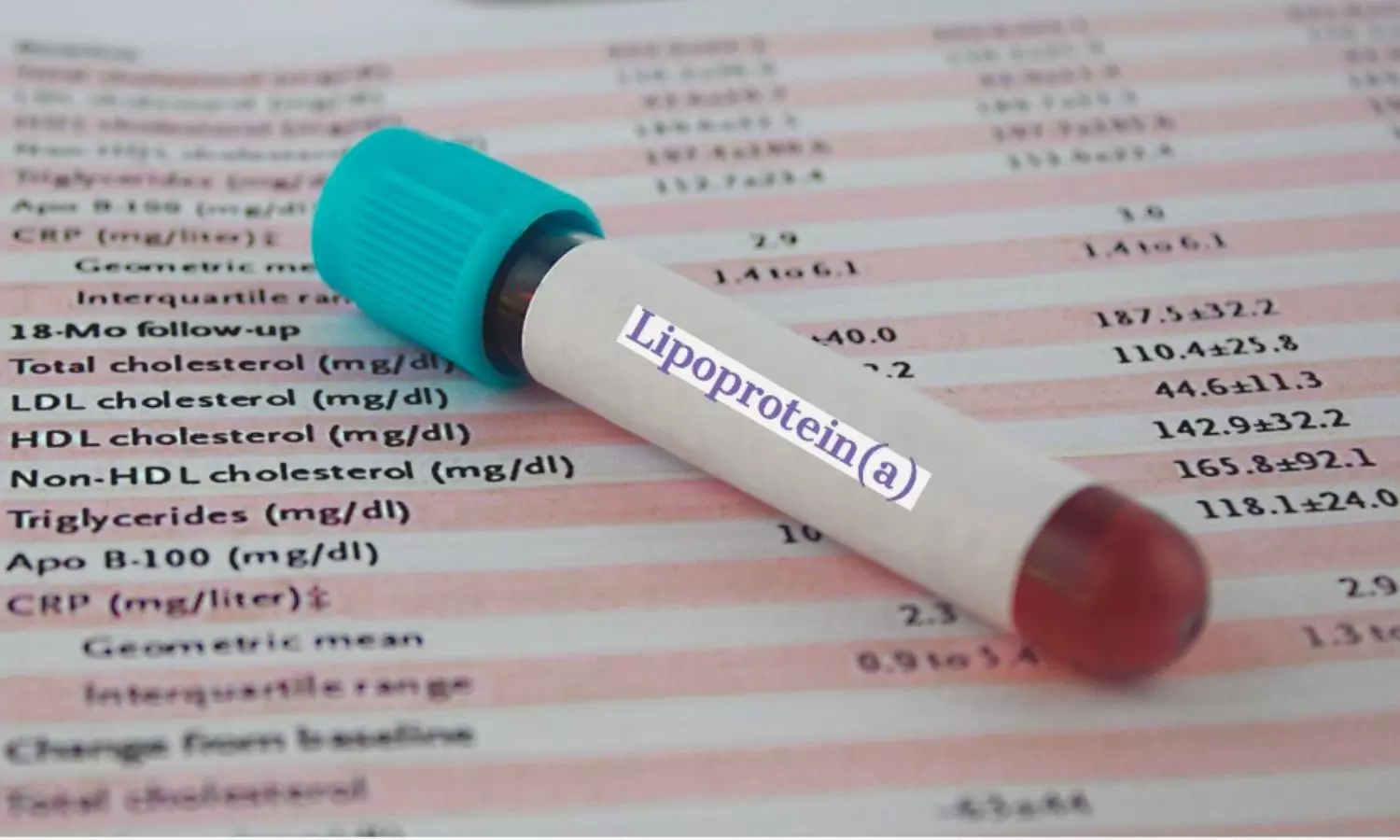
“When these cells resorb and form bone, they release certain substances into the blood that let us estimate how much bone turnover is going on at a given time,” she said.
These markers of bone resorption and formation follow a daily rhythm. The amplitude of this rhythm is larger for markers of bone resorption-which refers to the process of breaking down bones-than it is for markers of bone formation, she said.
“This rhythmicity is likely important for normal bone metabolism and suggests that sleep and circadian disturbance could directly affect bone health,” she said.
Researching the connection between sleep and bone health
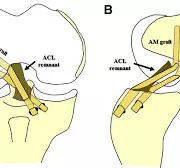
To further understand this relationship, Swanson and colleagues researched how markers of bone turnover responded to cumulative sleep restriction and circadian disruption.
For this study, participants lived in a completely controlled inpatient environment. The participants did not know what time it was, and they were put on a 28-hour schedule instead of a 24-hour day.
“This circadian disruption is designed to simulate the stresses endured during rotating night shift work and is roughly equivalent to flying four time zones west every day for three weeks,” she said. “The protocol also caused participants to get less sleep.”
The research team measured bone turnover markers at the beginning and end of this intervention and found significant detrimental changes in bone turnover in both men and women in response to the sleep and circadian disruption. The detrimental changes included declines in markers of bone formation that were significantly greater in younger individuals in both sexes compared to the older individuals.
In addition, young women showed significant increases in the bone resorption marker.
If a person is forming less bone while still resorbing the same amount-or even more-then, over time, that could lead to bone loss, osteoporosis, and increased fracture risk, Swanson said.
“And sex and age may play an important role, with younger women potentially being the most susceptible to the detrimental impact of poor sleep on bone health,” she said.