Injury prediction rule could decrease radiographic imaging exposure in children, study shows
Powered by WPeMatico
Powered by WPeMatico

Mumbai: The Neurosurgery department at Tata Memorial Centre (TMC), Mumbai, recently procured a state-of-the art intraoperative Ultrasound (iUS) machine for performing complex brain tumour surgeries.
The neurosurgery team at Tata Memorial Centre, led by Dr Aliasgar Moiyadi, has pioneered the application of iUS in India, and is one of the leading teams across the world. iUS is cost-efficient and with appropriate training, can become an important adjunct in the neurosurgeon’s armamentarium. The bKActiv machine, which was recently acquired by the department is the first installation of this advanced iUS system in the country.
Intraoperative imaging is crucial for safely and accurately removing intrinsic brain tumours. Combined with navigational aids (which is like a surgical GPS system), the iUS machine allows neurosurgeons to precisely track tumour remnants. Further, when combined with brain mapping techniques like awake surgery, they enable removal of tumours radically, even near critical functioning brain regions.
The system was unveiled on Saturday, 1st June 2024 at the Tata Memorial Hospital, Parel, Mumbai, in the presence of Dr Shailesh Shrikhande, Dy Director Tata Memorial hospital; Dr Aliasgar Moiyadi, Chief of Neurosurgery, Tata Memorial Centre; and Shri Chaitanya Sarawate, Managing Director, Wipro GE Healthcare South Asia, along with the entire departmental and operation theatre personnel.
Dr Moiyadi believes this advanced tool is likely to help his team and benefit the large number of brain tumour patients operated at the centre, many of whom are unable to access state-of-the-art care at subsidized rates elsewhere. iUS, being less costly than other intraoperative imaging systems (like intraoperative MRI), is particularly beneficial for resource constrained healthcare systems like ours.
The department has also led efforts to train neurosurgeons and equip them with the necessary skills to optimally perform iUS-guided surgeries, conducting training courses both in India as well as globally, hoping that more neurosurgeons can adopt this useful technique and disseminate the benefits to a larger number of patients across India. Dr A Moiyadi also pointed out that this equipment was procured with the aid of a generous grant provided by UBS.
He said that TMC is grateful for the support provided by UBS and highlighted the importance of such contributions, which strengthens TMC’s efforts of providing advanced cancer care for all Indians.
Speaking at the launch event, Shri Sarawate said, “We are committed to designing active imaging systems that help surgeons visualize anatomy and lesions, guide interventions, and navigate inside the human body – and this collaboration marks a significant milestone in advancing healthcare technology in India. Poised to revolutionize neurosurgery, the bkActiv Ultrasound system.
Powered by WPeMatico

Cambridge: AstraZeneca has announced the successful completion of the acquisition of Fusion Pharmaceuticals Inc., a clinical-stage biopharmaceutical company developing next-generation radioconjugates (RCs).
This acquisition complements AstraZeneca’s leading oncology portfolio with the addition of the Fusion pipeline of RCs, including their most advanced programme, FPI-2265, a potential new treatment for patients with metastatic castration-resistant prostate cancer (mCRPC), and brings new expertise and pioneering R&D, manufacturing and supply chain capabilities in actinium-based RCs to AstraZeneca. It also strengthens AstraZeneca’s presence in Canada, according to the release.
As a result of the acquisition, Fusion has become a wholly owned subsidiary of AstraZeneca, with operations in Canada and the US.
Radioconjugates (RCs) combine the precise targeting of antibodies, small molecules or peptides with potent medical radioisotopes to deliver radiation directly to cancer cells. By seeking out cancer cells, RCs provide a more precise mechanism of cancer cell killing compared with traditional radiation therapy, with the goal of improving efficacy while minimising toxicity on healthy cells. RCs are administered via systemic delivery, which enables their use in tumour types not accessible to external beam radiation and the targeting of cancer cells that have spread from the main tumour to other sites in the body.
Actinium-225 emits alpha particles and holds the promise of being a next-generation radioisotope in cancer treatment. By delivering a greater radiation dose over a shorter distance, alpha particles such as actinium-225 have the potential for more potent cancer cell killing, and targeted delivery, thereby minimising damage to surrounding healthy tissue.
Powered by WPeMatico
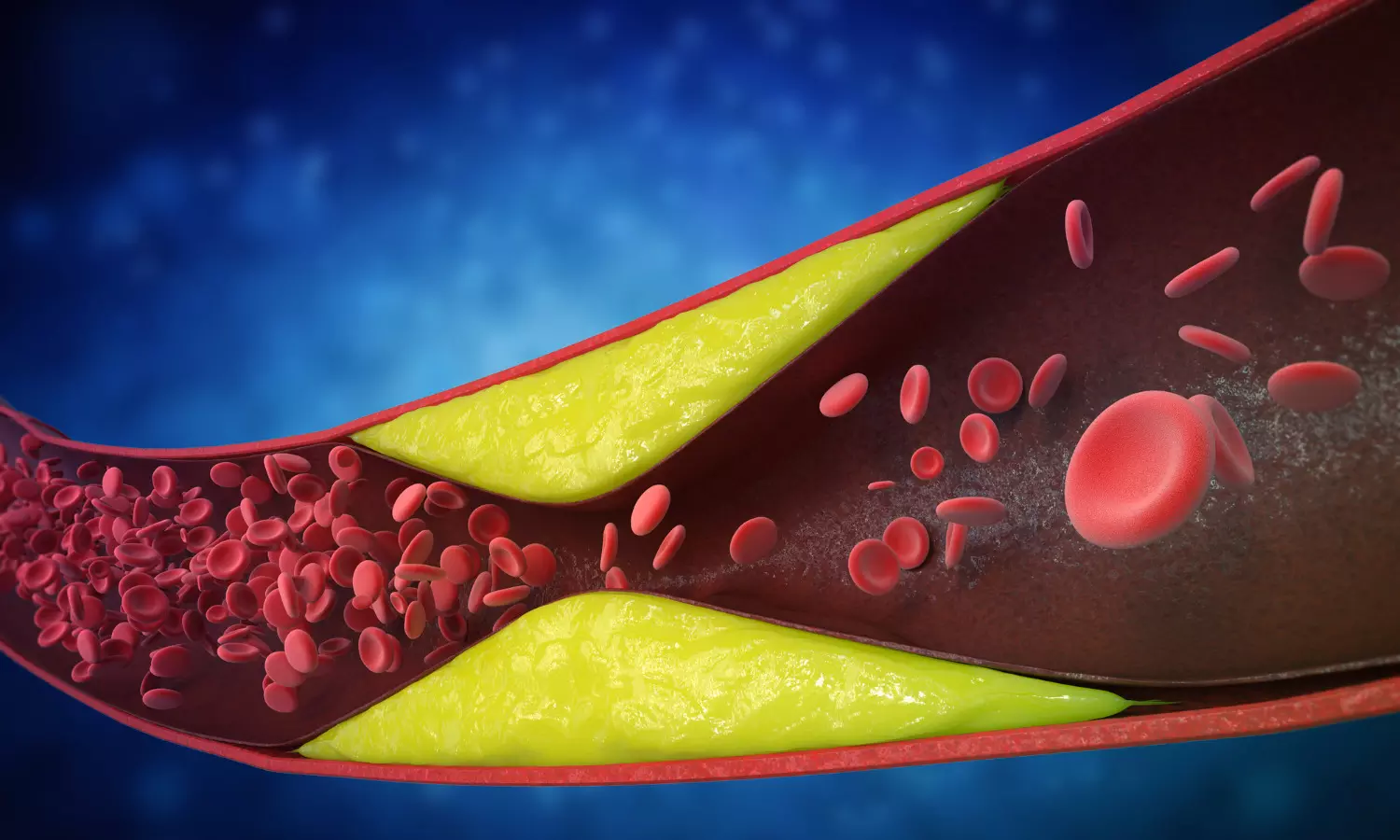
Positive results from a Phase I trial of AZD0780, an oral small molecule PCSK9 inhibitor administered on top of statin treatment, were presented at the European Atherosclerosis Society (EAS) in Lyon, France.
AZD0780 demonstrated a statistically significant reduction of 52% (95%CI: -57, -45) in LDL-C levels on top of rosuvastatin treatment, with 78% total reduction from baseline, in treatment-naive participants with hypercholesterolaemia.
The trial assessed the safety, tolerability, pharmacokinetics, and pharmacodynamics of AZD0780 in lowering low-density lipoprotein cholesterol (LDL-C) in plasma when administered as monotherapy and in combination with rosuvastatin.
Preliminary data comparing dosing with food versus fasting indicates dosing flexibility with regard to food.1 No serious adverse events were reported and AZD0780 was well tolerated.
AZD0780 progressed into Phase II trials in patients with dyslipidaemia earlier this year.
Sharon Barr, Executive Vice President, BioPharmaceuticals R&D, said: “The role of PCSK9 in cholesterol management is well established, and the compelling data generated with AZD0780 demonstrate the potential of this molecule for effective inhibition of this target and a possible next generation treatment for people with cardiovascular disease. AZD0780 inhibits PCSK9 via a novel, previously unexplored, mode of action that is compatible with traditional oral small molecule drug discovery. We are progressing development of AZD0780 as an innovative, convenient oral option for patients who are currently unable to meet their LDL-C targets with statins alone to reduce their risk of CV events.”
Elevated LDL-C levels in plasma is a key risk factor for cardiovascular disease and is estimated to cause 2.6 million deaths worldwide annually. Despite current treatment options, the global burden of dyslipidaemia is on the rise. More than 70% of patients with atherosclerotic cardiovascular disease (ASCVD) are still not achieving their LDL-C target, so there remains a vast unmet need among high risk patients for more varied and effective treatment options; achieving >70% LDL-C reduction could equate to >90% patients achieving LDL-C target levels according to guidelines.
AZD0780 is an oral, small molecule PCSK9 inhibitor that is being developed by AstraZeneca as a first-in-class therapy for patients with dyslipidaemia which cannot be controlled by statins alone. PSCK9 is a well-known and validated target in lipid metabolism and inhibiting PSCK9 signalling has shown to be effective in reducing LDL cholesterol levels in plasma.8 Lower LDL-C levels are associated with a reduction in the risk of long-term cardiovascular disease and major cardiovascular events.
The Phase I trial included participants receiving AZD0780 30 mg or 60 mg daily versus placebo (n=15 for each arm) for four weeks. An additional arm including 35 participants with hypercholesterolaemia (LDL-C >100 mg/dL to 190 mg/dL) received rosuvastatin 20 mg for three weeks followed by AZD0780 30 mg or placebo for four weeks.
Powered by WPeMatico
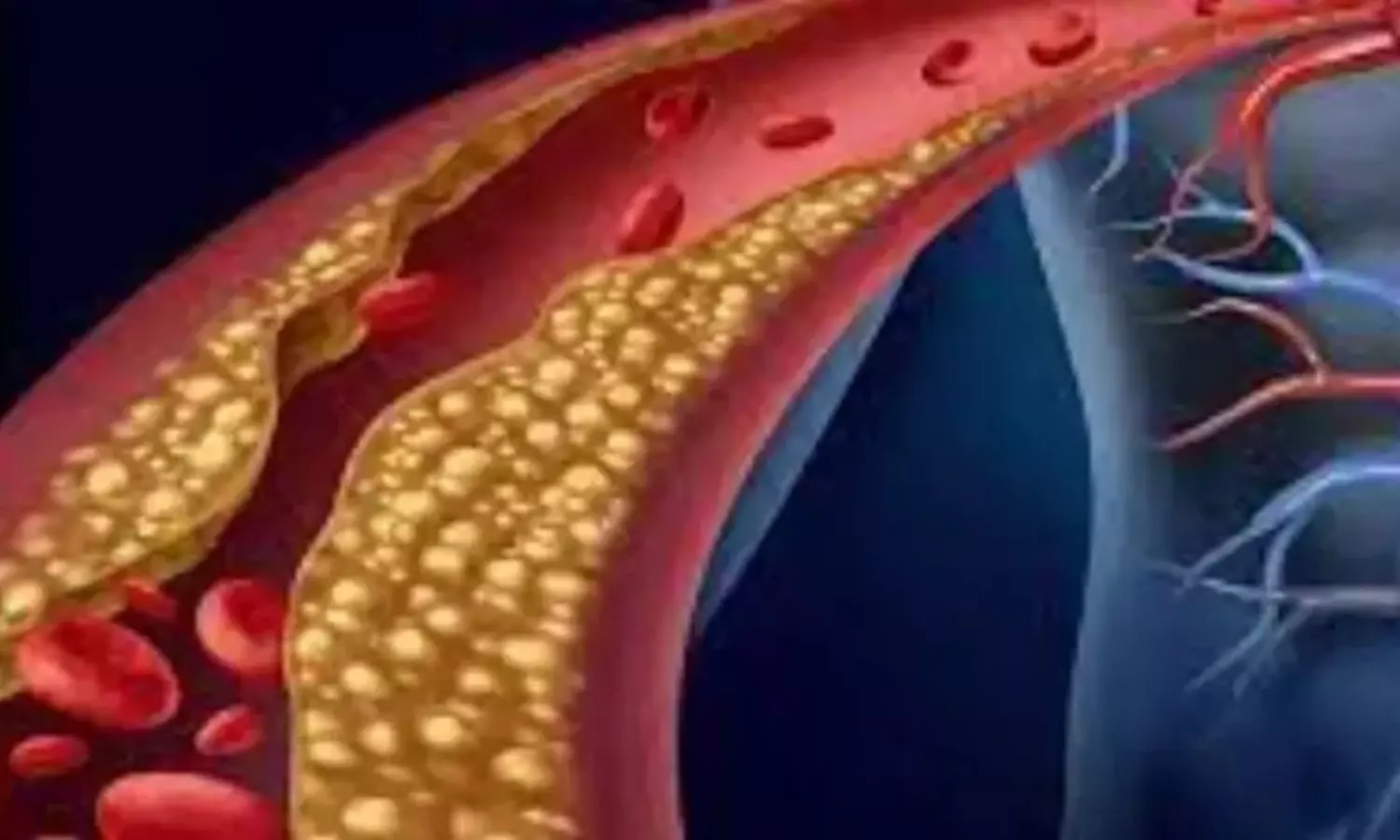
USA: In a groundbreaking development in lipid management, researchers have unveiled a promising RNA interference (RNAi) agent known as Plozasiran. This innovative therapeutic targets apolipoprotein C-III (APOC3), offering a potential game-changer for individuals grappling with mixed hyperlipidemia, a condition characterized by elevated levels of cholesterol and triglycerides.
The randomized, controlled trial (MUIR) involving participants with mixed hyperlipidemia showed that hyperlipidemia significantly reduced triglyceride levels at 24 weeks compared to placebo. The findings were published online in the New England Journal of Medicine on May 28, 2024.
Mixed hyperlipidemia poses a significant health risk, predisposing individuals to cardiovascular diseases, including heart attacks and strokes, due to an elevated non–high-density lipoprotein (HDL) cholesterol level, which is driven by remnant cholesterol in triglyceride-rich lipoproteins. While conventional treatments such as statins have proven effective in managing lipid levels, they often fall short in adequately addressing mixed hyperlipidemia, leaving a treatment gap that Plozasiran aims to fill.
The clearance and metabolism of triglyceride-rich lipoproteins are down-regulated through APOC3–mediated inhibition of lipoprotein lipase. Christie M. Ballantyne, Baylor College of Medicine and the Texas Heart Institute, Houston, and colleagues conducted a 48-week, phase 2b, double-blind, randomized, placebo-controlled trial evaluating the efficacy and safety of plozasiran, a hepatocyte-targeted APOC3 small interfering RNA, in patients with mixed hyperlipidemia (i.e., a triglyceride level of 150 to 499 mg per deciliter and either a LDL cholesterol level of ≥70 mg per deciliter or a non-HDL cholesterol level of ≥100 mg per deciliter).
The participants were assigned in a ratio of 3:1 to receive plozasiran or a placebo within each of the four cohorts (353 participants underwent randomization). In the first three cohorts, the participants received a subcutaneous plozasiran injection (10 mg, 25 mg, or 50 mg) or placebo on day one and week 12 (quarterly doses). In the fourth cohort, participants received 50 mg plozasiran or placebo on day one, and at week 24 (half-yearly dose).
The researchers pooled data from the participants who received a placebo. The primary endpoint was the percent change in fasting triglyceride level at week 24.
Based on the study, the researchers reported the following findings:
In conclusion, Plozasiran emerges as a beacon of hope for individuals grappling with mixed hyperlipidemia, offering a promising avenue for more effective lipid management. As the journey towards its approval and adoption progresses, the medical community eagerly anticipates the potential impact of this groundbreaking RNA interference agent on improving cardiovascular outcomes and enhancing patient well-being.
Reference:
Ballantyne CM, et al “Plozasiran, an RNA interference agent targeting APOC3, for mixed hyperlipidemia” N Engl J Med 2024; DOI: 10.1056/NEJMoa2404143.
Powered by WPeMatico

China: In a groundbreaking development in the field of diabetes prevention, the results of the FOCUS randomized clinical trial have unveiled the potential of Jinlida, a traditional Chinese medicine formulation, in mitigating the risk of diabetes among individuals with impaired glucose tolerance (IGT) and multiple metabolic abnormalities. This landmark study offers new insights into alternative approaches for diabetes prevention and management, particularly in populations at high risk of developing the condition.
The randomized clinical trial of 889 participants with IGT and multiple metabolic abnormalities showed that Jinlida granules (JLD) reduced the incidence of diabetes compared with placebo.
“After a median follow-up of 2.20 years, the JLD group had a significantly lower risk of developing diabetes than the placebo group,” the researchers reported in JAMA Internal Medicine.
Previous studies have shown that Jinlida granules, an approved treatment for type 2 diabetes in China, can reduce blood glucose levels, reduce glycated hemoglobin (HbA1c), and improve insulin resistance in people with type 2 diabetes. Hangyu Ji, Guang’anmen Hospital China Academy of Chinese Medical Sciences, Beijing, China, and colleagues aimed to evaluate the impact of long-term administration of JLD versus placebo on the incidence of diabetes in participants with IGT and multiple metabolic abnormalities.
For this purpose, the researchers conducted the FOCUS trial across 35 centers in 21 cities in China from 2019 to 2023. It enrolled individuals aged 18 to 70 years with IGT and multiple metabolic abnormalities
Participants were enrolled in a 1:1 ratio to receive JLD or placebo (9 g, 3 times per day, orally). They continued this regimen until they developed diabetes, were lost to follow-up, withdrew from the study, or died.
The primary outcome was diabetes occurrence, which was determined by two consecutive oral glucose tolerance tests. Secondary outcomes included waist circumference; HbA1c; fasting insulin level; fasting and 2-hour postprandial plasma glucose levels; homeostatic model assessment for insulin resistance (HOMA-IR); ankle-brachial index; total cholesterol, low-density lipoprotein cholesterol, and triglyceride levels; and carotid intima-media thickness.
The researchers reported the following findings:
· 889 participants were randomized, of whom 885 were in the full analysis set (442 in the JLD group; 443 in the placebo group; mean age, 52.57 years; 52.32% female).
· Following a median observation period of 2.20 years, participants in the JLD group had a lower risk of developing diabetes than those in the placebo group (hazard ratio, 0.59).
· During the follow-up period, the JLD group had a between-group difference of 0.95 cm in waist circumference, 9.2 mg/dL in 2-hour postprandial blood glucose level, 0.20% in HbA1c, 3.8 mg/dL in fasting blood glucose level, 6.6 mg/dL in total cholesterol level, 25.7 mg/dL in triglyceride levels, 4.3 mg/dL in low-density lipoprotein cholesterol level, and 0.47 in HOMA-IR compared with the placebo group.
· After 24 months of follow-up, the JLD group had a significant improvement in ankle-brachial index and waist circumference compared with the placebo group.
“The findings suggest that JLD can reduce diabetes risk in participants with IGT and multiple metabolic abnormalities,” the researchers concluded.
Reference:
Ji H, Zhao X, Chen X, et al. Jinlida for Diabetes Prevention in Impaired Glucose Tolerance and Multiple Metabolic Abnormalities: The FOCUS Randomized Clinical Trial. JAMA Intern Med. Published online June 03, 2024. doi:10.1001/jamainternmed.2024.1190
Powered by WPeMatico

Researchers have found that COVID-19 vaccines did not significantly reduce the incidence of cardiopulmonary events in high-risk cardiovascular patients, according to a secondary analysis of a randomized clinical trial. This study was published in JAMA Network Open, conducted by Fonseca, and colleagues investigated the efficacy of COVID-19 vaccines in preventing major adverse cardiovascular events (MACE) and other cardiopulmonary outcomes in patients following an acute coronary syndrome (ACS).
COVID-19 vaccines have proven effective in reducing hospitalizations and deaths due to the virus. However, their impact on preventing cardiopulmonary events in patients with a high risk of cardiovascular incidents remains unclear. This secondary analysis aimed to address this gap by utilizing data from the Vaccination Against Influenza to Prevent Cardiovascular Events After Acute Coronary Syndromes (VIP-ACS) trial.
The study was approved by the Comitê de Ética em Pesquisa-Hospital Israelita Albert Einstein, with informed written consent from all participants. It adhered to the CONSORT reporting guideline. The VIP-ACS trial, a multicenter study conducted between July 2019 and November 2020, assessed the efficacy of influenza vaccination post-ACS. For this analysis, researchers compared cardiopulmonary events between patients who received at least one COVID-19 vaccine dose and those who did not.
Participants were classified as COVID-19 vaccinated upon receiving at least one dose and subsequently censored from the unvaccinated group. To minimize immortal bias, a landmark analysis excluded patients with end points within 90 days of randomization.
End points included all-cause death, myocardial infarction, stroke, hospitalization for unstable angina, hospitalization for heart failure, urgent coronary revascularization, or hospitalization for respiratory infections. Secondary end points consisted of major adverse cardiovascular events (MACE). Adjusted Cox proportional hazard models were used for analysis, considering a P < .05 as significant.
• The study included 1,801 participants, with a median age of 56.7 years and 30.3% female.
• Among them, 292 individuals had a prior myocardial infarction, and 35.7% were active smokers.
• Of the 1,665 individuals who did not have cardiopulmonary events within the first 90 days, 50.2% received at least one COVID-19 vaccine dose.
• Most received the Oxford/AstraZeneca (ChAdOx1) viral vector vaccine.
• In the 90-day event-free follow-up analysis, the incidence of the primary end point was 9.37 events per 100 patient-years for unvaccinated individuals versus 4.81 events for vaccinated individuals (adjusted hazard ratio [aHR], 0.41; 95% CI, 0.18-0.94; P = .12).
• Vaccination did not significantly reduce MACE (aHR, 0.32; 95% CI, 0.07-1.53; P = .60), all-cause death (aHR, 0.29; 95% CI, 0.09-0.91; P = .12), or cardiovascular death (aHR, 0.42; 95% CI, 0.04-4.02; P > .99).
• A sensitivity analysis revealed similar findings: the adjusted incidence of the primary composite endpoint was (aHR, 0.43; 95% CI, 0.02-0.94; P = .12), and all-cause death was (aHR, 0.30; 95% CI, 0.10-0.89; P = .12).
In this analysis, receiving at least one COVID-19 vaccine dose post-ACS did not significantly affect the rates of primary composite end points or MACE compared to unvaccinated patients. This contrasts with retrospective studies indicating a short-term reduction in MACE risk post-COVID-19 vaccination.
COVID-19 vaccination did not significantly reduce cardiopulmonary events or major adverse cardiovascular events in high-risk cardiovascular patients post-ACS. These results highlight the need for further research to understand the role of COVID-19 vaccines in this population. Despite these findings, the study’s limitations, including non-randomization for COVID-19 vaccines and insufficient statistical power, suggest caution in generalizing the results.
Reference:
Fonseca, H. A. R., Damiani, L. P., Monfardini, F., Zimerman, A., Rizzo, L. V., & Berwanger, O. (2024). COVID-19 vaccination and cardiopulmonary events after acute coronary syndromes: A secondary analysis of a randomized clinical trial. JAMA Network Open, 7(5), e2413946. https://doi.org/10.1001/jamanetworkopen.2024.13946
Powered by WPeMatico

A new study by researchers from Arizona State University and their colleagues highlights a dietary strategy for significant health improvement and weight management.
Participants following an intermittent fasting and protein-pacing regimen, which involves evenly spaced protein intake throughout the day, saw better gut health, weight loss and metabolic responses. These benefits were notably greater than those seen with simple calorie restriction.
The findings, reported today in the journal Nature Communications, could advance our understanding of the relationship between the gut microbiome and metabolism and improve strategies for managing obesity.
The researchers compared the effects of two low-calorie dietary interventions: a heart-healthy continuous calorie-restricted diet (based on USDA dietary recommendations), and a calorie-restricted regimen incorporating intermittent fasting and protein pacing.
The trial was conducted with 41 individuals who were overweight or obese over a period of eight weeks. Individuals in the intermittent fasting and protein-pacing group showed a decrease in symptoms of gastrointestinal problems and an increase in diversity of the gut microbiota compared with those in the calorie-restriction group.
The intermittent fasting protocol increased beneficial microbes in the gut that have been linked to a lean body type and improved overall health. Additionally, it increased the levels of certain proteins (cytokines) in the blood associated with weight loss, as well as amino acid byproducts that promote fat burning.
Intermittent fasting is an eating pattern that cycles between periods of fasting and eating. The method has recently gained popularity for its potential health benefits, including weight loss, improved metabolic health and enhanced brain function.
“Given the gut microbiota’s location and its constant interaction with the GI tract, we have been gaining a deeper understanding of its pivotal role in dietary responses these last several years,” says Alex Mohr, lead author of the new study. “While limited in duration and sample size, this comprehensive investigation-which included the analysis of the gut microbiome, cytokines, fecal short-chain fatty acids and blood metabolites-underscores the intricate interplay between diet, host metabolism and microbial communities.”
Mohr led the microbiome and molecular investigations, evaluating gut microbial composition, inflammatory molecules called cytokines, SCFAs (metabolites derived from dietary fiber, important for regulating energy balance) and the metabolome.
Mohr is a researcher with the Biodesign Center for Health Through Microbiomes at ASU. Rosa Krajmalnik-Brown, the center director, and researchers Devin Bowes, Karen Sweazea and Corrie Whisner are also contributors to the study.
Corresponding author Paul Anciero of the Department of Health and Human Physiological Sciences at Skidmore College led the clinical trial, which tracked weight loss and body composition.
The study also included contributions from ASU researchers Paniz Jasbi and Judith Klein-Seetharaman, with the School of Molecular Sciences, and Dorothy Sears and Haiwei Gu, with the College of Health Solutions.
The gut microbiome refers to the diverse community of microorganisms residing in the gastrointestinal tract, including bacteria, viruses, fungi and other microbes. Numbering in the many trillions of organisms, this complex ecosystem plays a crucial role in essential bodily functions and overall health.
The gut microbiome helps break down food, produce vitamins and promote the absorption of nutrients. It plays a role in the development and function of the immune system by protecting the body against harmful pathogens. Finally, the gut microbiome keenly regulates metabolism, impacting body weight, fat storage and insulin sensitivity.
Caloric restriction, intermittent fasting (limiting food consumption to certain windows on some days) and protein pacing (controlled protein intake at specific meals) have been shown to affect body weight and composition, but the effect of these dietary modifications on the gut microbiome has been unclear until now.
“A healthy gut microbiome is essential for overall health, particularly in managing obesity and metabolic diseases,” says Sweazea, the ASU principal investigator of this Isagenix-funded study. “The gut bacteria influence how we store fat, balance glucose levels and respond to hormones that make us feel hungry or full. Disruptions in the gut microbiota can lead to increased inflammation, insulin resistance and weight gain, underscoring the critical role of gut health in preventing and managing metabolic disorders.”
The clinical trial involved 27 female and 14 male participants who were overweight or obese. Participants were divided into two groups: one following the intermittent fasting and protein pacing regimen, and the other adhering to a heart-healthy, calorie-restricted diet. Both groups were monitored over eight weeks for changes in weight, body composition, gut microbiome composition and plasma metabolomic signatures.
Participants following the intermittent fasting and protein pacing regimen experienced a significant reduction in gut symptoms and an increase in beneficial gut bacteria, particularly from the Christensenellaceae family. The study also found these microbes are associated with improved fat oxidation and metabolic health. In contrast, the calorie-restricted group showed an increase in metabolites linked to longevity-related pathways.
Despite both groups having similar average weekly energy intake, the intermittent fasting and protein pacing group achieved greater weight loss and fat reduction with an average loss of 8.81% of their initial body weights during the study. In comparison, those on a calorie-restricted diet lost an average of 5.4% body weight.
Participants who followed the intermittent fasting and protein-pacing diet experienced reductions in overall body fat, including belly fat and deep abdominal fat, and saw an increase in the percentage of lean body mass.
The study underscores the potential of intermittent fasting and protein-pacing diets in improving gut health and weight management. While further research is necessary, these findings offer a promising avenue for creating effective dietary interventions for obesity and related metabolic disorders.
“By identifying shifts in specific microbes, functional pathways and associated metabolites, this line of work holds promise for personalized health strategies as we can better tailor nutritional regimens to enhance gut function and metabolic outcomes,” Mohr says.
Reference:
Mohr, A.E., Sweazea, K.L., Bowes, D.A. et al. Gut microbiome remodeling and metabolomic profile improves in response to protein pacing with intermittent fasting versus continuous caloric restriction. Nat Commun 15, 4155 (2024). https://doi.org/10.1038/s41467-024-48355-5.
Powered by WPeMatico
USA: A recent five-year national retrospective cohort study has shed light on significant disparities in outcomes and healthcare utilization for diabetic ketoacidosis (DKA) among patients with type 1 and type 2 diabetes mellitus. The findings underscore the need for tailored management approaches and targeted interventions to address these disparities effectively.
The study revealed a higher mortality rate for patients with type 2 diabetes (T2D) hospitalized for ketoacidosis versus those with type 1 diabetes (T1D).
The mortality rate for those with T2D and diabetic ketoacidosis came in at 0.85% versus 0.2% for those with T1D and DKA, Shellsea Portillo Canales, MD, of St. Louis University Hospital reported.
The findings, presented at the American Association of Clinical Endocrinology, suggest the need for targeted healthcare strategies to address these disparities and improve patient outcomes, stressing the importance of personalized care approaches tailored to the specific needs of patients with different diabetes types.
Diabetic ketoacidosis is a serious and potentially life-threatening complication of diabetes, characterized by high blood sugar levels, ketone accumulation, and acidosis. While it is more commonly associated with type 1 diabetes, cases among individuals with type 2 diabetes have been increasingly reported in recent years.
The research team aimed to compare the impact of diabetes types on length of stay (LOS), mortality, and hospital charges.
For this purpose, they conducted a retrospective cohort study utilizing the 2016-2020 National Inpatient Sample (NIS) HCUP Database with adult patients admitted to acute care. Patients were divided into two cohorts, those with type 1 vs type 2 DM.
The primary endpoint was mortality obtained with multiple logistic regression analysis. Secondary endpoints included total hospital charges, and LOS assessed with multiple linear regression analysis. Missing data was accounted for with multiple imputation analyses. Multiplicity was addressed using statistical significance adjusted with Bonferroni-corrected alpha value.
The researchers reported the following findings:
As efforts to combat diabetes and its complications continue, studies like this play a crucial role in informing evidence-based interventions and policies aimed at reducing disparities and improving outcomes for all individuals affected by this chronic condition.
Reference:
Portillo Canales S, et al “Disparities in outcomes and healthcare utilization for diabetic ketoacidosis among patients with type 1 and type 2 diabetes mellitus: A five-year national retrospective cohort study” AACE 2024.
Powered by WPeMatico
Aneuploidy (the presence of an abnormal number of chromosomes) in embryos is a major cause of impaired embryo development, leading to conditions such as Down syndrome, as well as to pregnancy loss. The transfer of such embryos in women undergoing IVF is therefore usually avoided because of unfavourable pregnancy outcomes. But mosaic embryos, comprising both genetically normal and abnormal cells, can result in perfectly normal babies. Now, researchers have been able to understand how these mosaic embryos self-correct to develop normally. This understanding will improve the numbers of embryos suitable for transfer in women undergoing IVF, they say.
Presenting their results to the annual conference of the European Society of Human Genetics today (Monday), Ms Sheila Kwok, a PhD candidate in the Physiology Department of the University of Toronto, Toronto, Canada, will explain how the existence of a self-correction mechanism in mosaic embryos is consistent with the results of a large-scale clinical study of over 3500 pregnancy outcomes from mosaic embryo transfers from the International Registry of Mosaic Embryo Transfers (IRMET)* – where only 1.2% of preimplantation mosaicism persisted throughout pregnancy or postnatally. These findings, in turn, will reduce the stress on patients who have only mosaic embryos available for transfer, they say.
There has been an increasing number of women postponing motherhood over the past two decades. As they age, they become more likely to produce genetically abnormal embryos, due to higher error rates during egg development. This poses a challenge for women wishing to balance reproductive health with motherhood, since in IVF genetically normal embryos are prioritised for transfer to shorten time to pregnancy and reduce miscarriage and abnormal pregnancies. In older women, this can be very limiting, and therefore mosaic embryos are often the only available choice. Understanding how and which mosaic embryos will develop normally is therefore of ultimate importance.
“From earlier work carried out at the CReATe Fertility Centre, Toronto by Drs Clifford Librach and Mitko Madjunkov, we knew that mosaic embryos could result in ongoing pregnancies and live births at a rate of around 30%, which is lower than those from embryos with normal number of chromosomes (euploid embryos). This enabled us to start using mosaic embryos for transfer where no euploid embryos were available, but we still did not fully understand the process by which they self-corrected,” says Ms Kwok.
All pregnancies, natural or assisted, have around 3% risk of having an abnormal child. The 1.2% persistence of mosaicism therefore does not exceed this risk but prompts researchers to continue searching for answers. “We will expand our research to look at embryos with specific chromosomal aberrations to understand if this clearance mechanism is specific to the chromosome being affected,” says Ms Kwok. And, for all women who have a mosaic embryo transfer, current recommendations are prenatal testing and close pregnancy monitoring.”
By utilising advanced single-cell transcriptomic analysis1 and post-implantation embryo culturing systems, the researchers have now been able to address how two cell populations with differential fitness levels are able to co-exist in the same environment, and what are the mechanisms inducing the depletion of the abnormal cells. Their findings pointed to the fact that abnormal cells were less able to survive than normal cells, which had higher fitness. They now plan to use gene editing technology with stem cell-derived embryo models to validate the importance of the genes and molecular functions they have identified in these processes. In the future, they will apply small molecule treatments2 on mosaic embryos to try to facilitate this self-correction process.
“Embryology and assisted reproductive technologies have come a long way from the initial success rates of around 10-20%. In the last 10 years with advanced genetic tests for embryo selection rates have been close to 50-60%”, says Dr Svetlana Madjunkova MD, PhD, Head of Reproductive Genetics at CReATe Fertility Centre, the senior author of this work and the founder of IRMET. “But we still need to improve our understanding of which embryos to prioritise for transfer, to optimise patient treatment, help patients achieve their family goals and prevent the waste of time and resources, not to mention patient emotional and psychological stress, involved in transferring embryos that are not viable, and the complications associated with multiple embryo transfer. Our results, elucidating some of the mechanisms controlling normal embryo development, are providing strong evidence to believe that we have made an important step down this path.”
Professor Alexandre Reymond, from the Center for Integrative Genomics, University of Lausanne, Lausanne, Switzerland, and chair of the conference, said: “Juggling career and parenthood is difficult and often induces couples to become parents are an older age. While this increases genetic risk, we are now beginning to understand how to mitigate it.”
Reference:
Understanding how abnormal embryos self-correct may provide women with a better chance of IVF pregnancy, European Society of Human Genetics, Meeting: European Society of Human Genetics annual conference.
Powered by WPeMatico
