It’s time to use TikTok to talk to young people about obesity, says researcher
Powered by WPeMatico
Powered by WPeMatico

Kenvue, the producer of Tylenol said on Monday that Johnson & Johnson will be selling off its remaining 9.5% stake in the company. This decision follows roughly one year after the healthcare conglomerate separated and listed its consumer health business.
Based on Kenvue stock’s last close, the offering of 182.3 million shares would be worth about $3.75 billion, according to Reuters calculation.
Powered by WPeMatico

New Delhi: In a profound demonstration of courage and compassion, the family of a 76-year-old road accident victim has extended the gift of life to a 30-year-old man suffering from liver cirrhosis. This act, facilitated by the skilled medical team at Fortis Hospital Shalimar Bagh, Delhi, stands as a testament to the profound impact of organ donation.
Dr Sonal Gupta, Director, and HOD Neurosurgery at Fortis Hospital Shalimar Bagh, recounted the harrowing circumstances that led to the organ donation.
According to a PTI report, a 28-km green corridor in the national capital was created from Shalimar Bagh to Saket to transport a liver to save the life of a 30-year-old man battling liver cirrhosis.
The elderly man died on May 3 and a green corridor set up to transport his liver reached Max Hospital, Saket in 44 minutes, according to a statement.
Also Read:16.7 kgs gunny bag tumour removed from 27-year-old man’s back at FMRI Gurugram
“Despite the emergency intervention, the patient suffered brain haemorrhage due to the gravity of the head injury following the accident and multiple clots in the brain. Sadly, he could not be revived despite critical care interventions and ventilator support,” Gupta said, reports news agency ANI.
“We salute the deceased donor and deeply appreciate the generosity of his family in recognizing the value of organ donation and giving the gift of life to those in need. The seamless collaboration between our dedicated doctors and the police made this life-saving donation possible. We hope this heartwarming example inspires more people to register for organ donation and make a difference,” she added.
According to the doctors, the road accident victim after the incident was rushed to Fortis Shalimar Bagh hospital with severe head injury and oral bleeding in the first week of May. On admission, the patient was conscious, but within, half an hour he lost consciousness due to a rapidly enlarging clot in the brain. An urgent CT scan of the head revealed a large clot (Subdural Hematoma) in the brain.
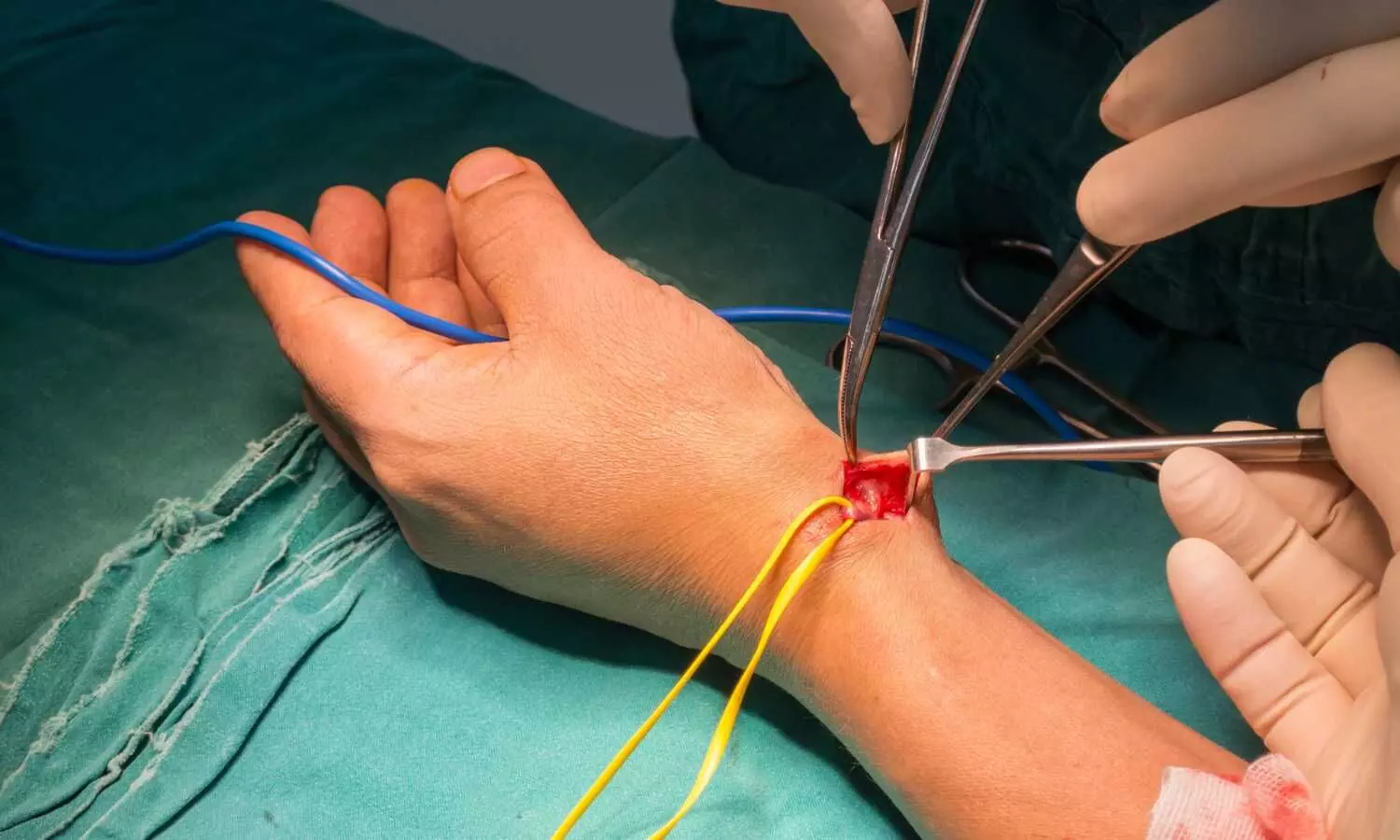
An emergency brain surgery was conducted to remove the clot and bone on the right side of the skull to create extra space for the swollen injured brain. After the surgery, he was placed in the ICU on a ventilator, where a multi-disciplinary team of doctors provided intensive care. Despite vigorous efforts and medications to reduce brain swelling, the victim unfortunately succumbed to his injuries.
Amidst profound sorrow and grief, the family of the deceased displayed courage and generosity by consenting to donate their loved one’s liver to a 30-year-old man suffering from liver cirrhosis. The entire process of multi-organ retrieval surgery took around 2 hours and 35 minutes. A green corridor to transport the liver was created from Fortis Shalimar Bagh to Max Hospital, Saket covering a distance of 28.4 km in just 44 minutes.
Deepak Narang, Facility Director at Fortis Hospital Shalimar Bagh, expressed gratitude towards the donor’s family and emphasized the importance of organ donation in saving lives.
“We remain indebted to the family for their magnanimity amid grief. The clockwork precision of all internal and external medical teams made this donation a reality. This should encourage more people to come forward and get themselves registered for organ donation to save more lives,” Narang said.
According to NOTTO (National Organ and Tissue Transplant Organization), once a patient is declared brain dead, the hospital can counsel the family for organ donation. NOTTO protocol and guidelines stipulate that the treating hospital provide all details and obtain necessary clearances for a possible organ donation. In this case, the No Objection Certificate in a Medico-Legal Case (NOC-MLC) was obtained and a request for a green corridor was made.
According to an ANI report, It is estimated that almost 5 lakh Indians face organ failure every year and only 2-3 percent receive a life-saving transplant. As per data available with NOTTO, in 2022, 11 cadaver donations have been made with the successful retrieval of 30 organs in Delhi.
Every year, hundreds of people die in India, waiting for an organ transplant. Due to a lack of awareness and misconceptions, there is a shortage of organ donors, and with each passing year, the gap between the number of organs donated and the number of people waiting for transplants is growing wider. Timely cadaveric organ donation can save many lives and more people would come forth and pledge their organs if they receive more information and are educated on the benefits of organ donation.
Powered by WPeMatico

India: Melasma, a common skin condition characterized by hyperpigmentation, has long been a challenge to treat effectively. However, a recent study published in the International Journal of Dermatology has sparked hope by investigating the use of oral melatonin as a potential therapy for recalcitrant cases of melasma. The findings of this research offer a promising glimpse into a novel approach to managing this stubborn dermatological condition.
The study suggests considering oral melatonin as a well-tolerated off-label treatment for patients with recalcitrant melasma, although additional research is required.
Melasma, referred to as the “mask of pregnancy,” typically manifests as dark patches on the face, particularly on the cheeks, forehead, and upper lip. While various topical treatments and procedures exist, recalcitrant cases—those resistant to conventional therapies—present a significant clinical dilemma for dermatologists and patients alike.
The study conducted by Rashmi Sarkar, Lady Hardinge Medical College and Maulana Azad Medical College, New Delhi, India, and colleagues aimed to evaluate the efficacy of oral melatonin supplementation in reducing the severity of melasma and improving patients’ quality of life.
Melatonin, a hormone primarily known for its role in regulating sleep-wake cycles, has garnered increasing attention for its potential antioxidant and anti-inflammatory properties. Researchers hypothesized that oral melatonin supplementation could modulate melanogenesis, the process by which melanin is produced in the skin, thereby mitigating hyperpigmentation associated with melasma.
The researchers presented data from 7 patients with recalcitrant melasma treated with oral melatonin. All patients previously received treatment with either topical creams, including topical combination cream, oral tranexamic acid, or chemical peels without significant improvements.
Following a 4-week washout period, all patients received daily 3-mg melatonin tablets and used sunscreen for 12 weeks. All patients reported lightening of pigmentation, and there was an improvement from baseline in the Melasma Area and Severity Index scores.
The findings underscore the potential of oral melatonin as a safe and effective adjunctive therapy for individuals struggling with stubborn melasma. By harnessing melatonin’s antioxidant and anti-inflammatory properties, dermatologists may have a valuable tool in their arsenal for addressing this challenging condition.
While further research is needed to elucidate the optimal dosage, duration, and long-term effects of oral melatonin supplementation in melasma management, the study represents a significant step forward in expanding treatment options for patients with recalcitrant cases.
In conclusion, the investigation into the use of oral melatonin in recalcitrant melasma offers renewed hope for individuals seeking relief from this distressing skin condition. As dermatologists continue to explore innovative therapeutic approaches, oral melatonin stands out as a promising avenue for improving outcomes and enhancing the quality of life for those affected by melasma.
Reference:
Sarkar, R., Verma, B., & Mendiratta, V. Use of oral melatonin in recalcitrant melasma. International Journal of Dermatology. https://doi.org/10.1111/ijd.17201
Powered by WPeMatico

Italy: In a landmark randomized clinical trial, researchers have delved into a crucial aspect of cardiac care: the optimal approach to revascularization in older patients experiencing myocardial infarction (MI) and possessing a high risk of bleeding. The study, published in JAMA Cardiology, sheds light on a debate that has long perplexed cardiologists and aims to provide clarity for practitioners and patients alike.
The prespecified analysis of the FIRE randomized clinical trial (RCT), including 1445 patients, revealed that high bleeding risk (HBR) status was common in older patients with MI, and is correlated with a significant rise in ischemic and bleeding complications risk. Physiology-guided complete revascularization effectively improves outcomes and reduces complication rate, regardless of HBR status.
Based on the findings, the researchers suggest that HBR status alone should not deter applying physiology-guided complete revascularization in older patients with MI and multivessel disease.
Myocardial infarction, commonly known as a heart attack, is a life-threatening condition characterized by a blood flow blockage to the heart muscle. Revascularization, blood flow restoration to the affected area, is a cornerstone of treatment. However, the optimal extent of revascularization has been a subject of ongoing debate, particularly in older patients with additional risk factors such as a high propensity for bleeding.
Patients with high bleeding risk have a poor prognosis, and whether they may benefit from complete revascularization after myocardial infarction is not known. Considering this, Andrea Erriquez, Cardiology Unit, Azienda Ospedaliero Universitaria di Ferrara, Ferrara, Italy, and colleagues aimed to investigate the benefit of physiology-guided complete revascularization versus a culprit-only strategy in patients with HBR, MI, and multivessel disease.
FIRE was an investigator-initiated, open-label, multicenter trial. Researchers enrolled patients aged 75 years or older with MI and multivessel disease at 34 European centers from 2019 to 2021. Physiology treatment was performed either by angiography- or wire-based assessment. Patients were divided into HBR or non-HBR categories per the Academic Research Consortium HBR document.
Patients were randomized to either physiology-guided complete revascularization or culprit-only strategy.
The primary outcome comprised a composite of death, stroke, MI, or revascularization at one year. Secondary outcomes included a composite of MI or cardiovascular death and Bleeding Academic Research Consortium (BARC) types 3 to 5.
The following were the key findings of the study:
The findings suggest that HBR status was common in older patients with MI and was linked with a higher risk of ischemic and bleeding complications, including death. Physiology-guided complete revascularization emerged as an effective method to reduce ischemic complications, including myocardial infarction and cardiovascular death, and should be considered in treating patients with HBR.
In conclusion, the randomized clinical trial comparing complete versus culprit-only revascularization in older patients with myocardial infarction and high bleeding risk represents a significant advancement in the field of cardiology. These findings are poised to inform guidelines and shape clinical practice, ultimately improving the quality of care for individuals navigating the complexities of cardiovascular disease.
Reference:
Erriquez A, Campo G, Guiducci V, et al. Complete vs Culprit-Only Revascularization in Older Patients With Myocardial Infarction and High Bleeding Risk: A Randomized Clinical Trial. JAMA Cardiol. Published online May 08, 2024.
doi:10.1001/jamacardio.2024.0804
Powered by WPeMatico

A recent research conducted as part of the Strong Heart Family Study (SHFS) and the Multi-Ethnic Study of Atherosclerosis (MESA) unveiled a concerning association between arsenic levels in water and the incidence of Type 2 Diabetes (T2D) within American Indian and diverse urban communities in the United States. The findings were published in the Diabetes Care journal.
This study examined data from a total of 1,791 participants in SHFS and 5,777 participants in MESA to assess the impact of arsenic exposure from both federally regulated community water systems (CWSs) and unregulated private wells on T2D incidence. The participants were free of T2D at the beginning of the study between 2000 and 2003 and were followed over several years until 2010 for SHFS and 2019 for MESA.
The findings revealed that the T2D incidence rates were significantly influenced by arsenic levels in water. In the SHFS cohort, there were 24.4 cases per 1,000 person-years, while in MESA, the rate was 11.2 per 1,000 person-years. The meta-analysis encompassed both cohorts and observed that, for every doubling in arsenic concentration in CWS, the hazard ratio for T2D incidence increased by 10%. Similar patterns were observed for arsenic from private wells, although the association was weaker.
These findings suggest that even low to moderate levels of arsenic in water (defined as being below 10 µg/L) were linked to an increased risk of developing T2D. The association between arsenic exposure and T2D incidence was noted to be more pronounced among certain demographic groups. The individuals with a Body Mass Index (BMI) below 25 kg/m² and female participants expressed larger magnitude hazard ratios that suggests a increased vulnerability to the effects of arsenic on diabetes risk.
These findings underline the importance of monitoring and regulating arsenic levels in water sources. Access to clean and safe drinking water is a fundamental human right and efforts to reduce arsenic contamination should be prioritized to safeguard public health. It becomes increasingly evident that environmental factors play an important role in shaping health outcomes. We can take significant steps towards preventing and managing chronic diseases like Type 2 Diabetes by identifying and addressing these risk factors.
Source:
Spaur, M., Galvez-Fernandez, M., Chen, Q., Lombard, M. A., Bostick, B. C., Factor-Litvak, P., Fretts, A. M., Shea, S. J., Navas-Acien, A., & Nigra, A. E. (2024). Association of Water Arsenic With Incident Diabetes in U.S. Adults: The Multi-Ethnic Study of Atherosclerosis and the Strong Heart Study. In Diabetes Care. American Diabetes Association. https://doi.org/10.2337/dc23-2231
Powered by WPeMatico

USA: In a groundbreaking development for patients suffering from thyroid eye disease (TED), recent clinical trials have demonstrated the remarkable efficacy of Teprotumumab across various phenotypes of the condition. The findings, presented during an oral presentation at the American Association of Clinical Endocrinology, offer new hope to individuals grappling with the debilitating symptoms of this autoimmune disorder.
The new data from the post-hoc analysis suggests that teprotumumab (Tepezza) works equally well in older and younger patients with thyroid eye disease, irrespective of TED duration.
The researchers observed comparable improvements with teprotumumab among patients with age-related phenotypic I or II thyroid eye disease.
“At 24 weeks, 81% of patients with phenotypic I thyroid eye disease (younger than 40 years) and 73.7% of those with phenotypic II disease (40 and older) had overall improvements with teprotumumab, a difference that was not statistically significant,” Soheab Ugradar, MD, of Thrive Health in Beverly Hills, California, reported.
Results were comparable between the older and younger patients for diplopia, clinical activity score, proptosis, and Graves’ Ophthalmology Quality of Life score.
Thyroid eye disease, also known as Graves’ orbitopathy, is a distressing condition characterized by inflammation and swelling of the tissues around the eyes. It commonly affects individuals with thyroid disorders, particularly those with Graves’ disease, an autoimmune condition causing hyperthyroidism. TED can lead to significant visual impairment, disfigurement, and decreased quality of life for patients.
Phenotypic I thyroid eye disease involves orbital fat expansion and proptosis with minimal to no periorbital inflammation or diplopia, with low dysthyroid optic neuropathy. Phenotypic II thyroid eye disease involves extraocular muscle enlargement and fibrosis, periorbital inflammation, and diplopia, with higher dysthyroid optic neuropathy rates.
Teprotumumab, a monoclonal antibody developed by Horizon Therapeutics, has emerged as a promising therapeutic option for individuals battling TED. The drug works by targeting the insulin-like growth factor 1 receptor (IGF-1R), which plays an important role in the pathogenesis of the disease. By inhibiting IGF-1R signaling, Teprotumumab effectively reduces inflammation and tissue expansion around the eyes.
For this analysis, Ugradar and the team identified patients in the randomized OPTIC trial and the open-label OPTIC-X trial, in which patients received eight infusions of teprotumumab.
The study comprised 121 patients, 22 with phenotypic 1 disease and 99 with phenotypic 2 disease. The mean age for patients with type I disease was 32.8, 59.1% were women, the mean time since diagnosis was 8.6 months, and the mean clinical activity score was 4.1. For the patients with type II disease, the mean age was 54.5, 72.7% were women, the mean clinical activity score was 4.8, and the mean time since diagnosis was 7.7 months.
The following were the key findings of the study:
The promising results of these clinical trials have ignited excitement within the medical community and among patients alike. With Teprotumumab poised to become a cornerstone of thyroid eye disease management, individuals grappling with this challenging condition can look forward to improved outcomes and enhanced quality of life. As further research unfolds, the potential of this groundbreaking therapy to transform the landscape of TED treatment appears increasingly tangible.
Reference:
Ugradar S, et al “Efficacy of teprotumumab in phenotype I vs type II thyroid eye disease” AACE 2024.
Powered by WPeMatico
USA: In a groundbreaking investigation into the comparative outcomes of radial versus femoral arterial access for percutaneous coronary intervention (PCI) in the United States, the study, published in the Journal of the Society for Cardiovascular Angiography & Interventions, has unveiled compelling insights into temporal trends and clinical implications. This pioneering research sheds new light on the evolving landscape of interventional cardiology and offers valuable guidance for healthcare practitioners and policymakers alike.
The study found a 2.8-fold increase in the use of radial access for PCI in the US over the past decade and represents the dominant form of access across all procedural indications. Based on instrumental variable analysis, a technique used to support causal inference, radial access was tied to lower in-hospital mortality, major access bleeding, and other major vascular complication rates than femoral access but with a slightly higher ischemic stroke risk.
New data presented at the Society for Cardiovascular Angiography & Interventions (SCAI) 2024 Scientific Sessions demonstrated the superiority of radial arterial access over femoral arterial access for coronary interventions.
Percutaneous coronary intervention (PCI), commonly known as angioplasty, is a minimally invasive procedure used to open blocked or narrowed coronary arteries, typically performed to treat coronary artery disease (CAD) and relieve symptoms of angina or prevent heart attacks. The choice of arterial access—radial (via the wrist) or femoral (via the groin)—has long been debatable among interventional cardiologists, with each approach carrying its own set of benefits and limitations.
Clinical practice guidelines recommend radial access for PCI because of superior outcomes compared with femoral access. Historically, the adoption of radial access in the United States has lagged behind much of the rest of the world, however, there is a lack of contemporary data on access site selection across the spectrum of clinical presentations and its association with outcomes.
To fill this knowledge gap, Reza Fazel, Beth Israel Deaconess Medical Center, Brookline, MA, and colleagues aimed to examine temporal trends in the utilization of radial versus femoral arterial access for PCI and to evaluate associated clinical outcomes.
For this purpose, the research team conducted a retrospective cohort study from the National Cardiovascular Data Registry’s CathPCI Registry, including PCIs performed between 2013 and 2022. They evaluated the comparative safety of radial versus femoral access for PCI using instrumental variable analysis exploiting operator variation in access preferences.
The following were the key findings of the study:
As the field of interventional cardiology continues to evolve, studies like this play a pivotal role in informing best practices and shaping the future of cardiovascular care. By leveraging real-world data and rigorous analysis, researchers aim to drive innovation and improve outcomes for patients undergoing percutaneous coronary intervention.
“The study demonstrates a sea change in which PCI is performed in the US in response to trial data but also highlights the continued opportunity for practice improvement with dramatic interoperator variation,” said Dr. Fazel.
“It confirms that the benefit observed for radial access in RCTs has also been seen in real-world practice, including the largest benefits for the highest-risk patients. Finally, it shows a highly credible novel finding on the increased stroke risk.
Reference:
DOI: https://doi.org/10.1016/j.jscai.2024.101866
Powered by WPeMatico

China: In a groundbreaking systematic review and meta-analysis, researchers have unveiled compelling evidence of the cardioprotective properties of curcumin against diabetic cardiomyopathies. Published in Phytomedicine journal, this study consolidates preclinical research findings, shedding light on curcumin’s therapeutic potential in managing cardiovascular complications associated with diabetes.
The study found that curcumin may exert cardioprotective effects in diabetic cardiomyopathy (DCM) through its anti-inflammatory, antioxidant, anti-apoptotic, and autophagy-enhancing effects. The protective effect of curcumin was found to be proportional to the dose, and the efficacy may be increased further at a concentration of above 200 mg/kg, and there is a need for further validation.
Diabetic cardiomyopathy (DCM) is a common complication of diabetes that often leads to further damage to the heart muscle. Curcumin has been proven to have various cardioprotective effects, however, no systematic review has been conducted on the protective effect against DCM.
Against the above background, Wujiao Wang, University of Chinese Medicine, Beijing, China, and colleagues aimed to analyze the preclinical (animal model) evidence of curcumin’s therapeutic effects in DCM.
For this purpose, the researchers searched eight databases and two registry systems from the time of library construction to 1 November 2023. Rigorous data extraction and quality assessment was performed. Using the SYRCLE RoB tool, the methodological quality of the included studies was appraised. Statistical analyses were carried out using RevMan 5.4 software, and Egger’s test and Funnel plots were performed using Stata 17.0 software to assess publication bias. This study included 32 trials with 681 animals.
Meta-analysis showed that curcumin significantly improved cardiac function indices (LVFS, LVEF, and LVSd), decreased markers of myocardial injury, HW/BW ratio, and randomized blood glucose compared to the control group, in addition to showing beneficial effects on mechanistic indices of inflammation, myocardial oxidation, apoptosis, and autophagy.
“Our study is the first meta-analysis of preclinical studies of curcumin for DCM treatment, and our results suggest that curcumin may play a cardioprotective role in DCM through its anti-inflammatory, antioxidant, autophagy-enhancing, and anti-apoptotic effects,” the researchers wrote.
The meta-analysis further elucidated the dose-dependent relationship between curcumin supplementation and its cardioprotective effects, providing valuable insights for future clinical studies and therapeutic applications.
As the prevalence of diabetes continues to escalate globally, the quest for effective strategies to prevent and manage diabetic complications becomes paramount. The findings of this systematic review offer compelling evidence supporting the therapeutic potential of curcumin in mitigating diabetic cardiomyopathies, paving the way for further research and clinical translation in cardiovascular medicine.
Reference:
Wang, W., Chang, P., Jin, J., Pu, F., Li, D., Bai, Y., Dong, K., Yang, Q., & Li, T. (2024). Cardioprotective effects of curcumin against Diabetic Cardiomyopathies: A systematic review and meta-analysis of preclinical studies. Phytomedicine, 129, 155619. https://doi.org/10.1016/j.phymed.2024.155619
Powered by WPeMatico

One in four patients with insulin-dependent diabetes aged 16 years and older also exhibit some kind of eating disorder symptoms, according to a recent meta-analysis conducted at the University of Eastern Finland. In addition to typical eating disorder symptoms, such as binge eating and food restriction, insulin-dependent diabetes is also associated with insulin omission, i.e., a unique form of disordered eating where insulin doses are intentionally restricted or skipped entirely due to fears of weight gain.
“Intentional skipping or restriction of insulin doses will lead to weight loss, but this also maintains high blood glucose, throwing the management of diabetes off balance,” Doctoral Researcher Pia Niemelä of the University of Eastern Finland says.
According to the meta-analysis, one in five patients reported intentional insulin omission.
Published in Eating Behaviors, the meta-analysis compiled findings from 45 previous studies. The data included a total of 11,592 individuals with insulin-dependent diabetes, of whom 2,521 exhibited eating disorder symptoms.
Eating disorder symptoms were more common in women than in men, which is an observation that has previously been made in young people as well. Age, however, was not a significant factor, as eating disorders occurred regardless of age group.
“Eating disorder symptoms are often thought to affect adolescents and young adults. However, our meta-analysis shows that adults, too, suffer from eating disorder symptoms, which is why it is important to learn to identify patients with eating disorders. Here in Finland, for example, we currently don’t have a care pathway for patients who have both diabetes and eating disorders. Understanding the clinical picture and its prevalence is the first step in developing treatment and care pathways,” Niemelä says.
Diabetics with eating disorder symptoms have a higher risk of comorbidities and complications associated with diabetes. Eating disorder symptoms are screened using various surveys, including the most commonly used DEPS-R, which in the current meta-analysis was positive in 27 per cent of the subjects.
Reference:
Pia E. Niemelä, Hanna A. Leppänen, Ari Voutilainen, Essi M. Möykkynen, Kirsi A. Virtanen, Anu A. Ruusunen, Reeta M. Rintamäki, Prevalence of eating disorder symptoms in people with insulin-dependent-diabetes: A systematic review and meta-analysis, Eating Behaviors, https://doi.org/10.1016/j.eatbeh.2024.101863
Powered by WPeMatico
