Black women in US murdered six times more often than White women between 1999 and 2020, finds state-level analysis
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Ahmedabad: Zydus Lifesciences Limited has received final approvals from the United States Food and Drug Administration (USFDA) to manufacture and market Dexamethasone Tablets USP, 0.5 mg, 0.75 mg, 1.5 mg, 4 mg and 6 mg (USRLD: Decadron Tablets) and Dexamethasone Tablets USP, 2 mg
(USRLD: Dexamethasone Tablets).
Dexamethasone is used to treat a number of different conditions, such as inflammation
(swelling), severe allergies, adrenal problems, arthritis, asthma, blood or bone marrow
problems, kidney problems, skin conditions, and flare-ups of multiple sclerosis.
The products
will be manufactured at the group’s formulation manufacturing facility at Baddi, Himachal
Pradesh.
Dexamethasone Tablets USP, 0.5 mg, 0.75 mg, 1.5 mg, 4 mg and 6 mg had annual sales of
USD 22 mn and Dexamethasone Tablets USP, 2 mg has annual sales of USD 6 mn in the
United States (IQVIA Dec. Nov. 2023).
The group now has 386 approvals and has so far filed over 448* ANDAs since the
commencement of the filing process in FY 2003-04.
Medical Dialogues team had earlier reported that Zydus Lifesciences had received final approval from the USFDA for Clindamycin Phosphate Gel USP, 1% (USRLD: Cleocin T Gel, 1%).
Read also: Zydus bags USFDA nod for acne gel Clindamycin Phosphate
Formerly known as Cadila Healthcare Limited, Zydus Lifesciences Limited is an Indian multinational pharmaceutical company headquartered in Ahmedabad. The company is primarily engaged in the production of generic drugs. Cadila was founded in 1952 by Ramanbhai Patel.
Powered by WPeMatico

Chandigarh- The Postgraduate Institute of Medical Education and Research (PGIMER) Chandigarh has issued a notice announcing the upcoming 3rd physical counselling/seat allotment for candidates who applied under the sponsored category for MD/MS admission at PGIMER Chandigarh and qualified for the INI-CET (January 2024) conducted by All India Institute of Medical Sciences (AIIMS) New Delhi.
As per the notice, the third Physical Counselling/Seat Allotment is scheduled for Thursday, February 15th, 2024, at 11:00 AM in the APC Auditorium at PGIMER, Chandigarh. Candidates must be sited in the auditorium by 10:45 AM on February 15th, 2024. Later, the seats to be filled in the third counselling will be uploaded on the PGIMER website on the evening of 11 February 2024.
Candidates are instructed to submit one set of photocopies of certain original documents from their respective employers at the time of counselling. If the candidates fail to submit the documents they will not be considered for admission.
The documents that need to be submitted are mentioned below-
1 10th class certificate.
2 MBBS Degree.
3 Internship Certificate.
4 State Medical Council/National Medical Commission Registration Certificate.
5 Original Sponsorship Certificate.
6 No Objection Certificate (NOC).
Previously, PGIMER had announced the provisional seat allocations for the second counselling of sponsored candidates for the January 2024 session. According to the announcements, there were a total of 8 courses with a total of 30 vacant seats in the courses. Meanwhile, the second counselling session was scheduled for January 19, 2024, at 11:00 AM in the Bhargava Auditorium, PGIMER, Chandigarh.
To view the notice, click the link below-
Powered by WPeMatico

Panaji: A doctor and three others allegedly assaulted a fellow customer at a restaurant in Old Goa and created a ruckus there, police said on Thursday.
The incident took place around 11 pm on February 7, following which a case was registered against the four persons, they said.
The accused were identified as Dr Ajeya Mundhekar, Shubham Sawant, Swapnil Naik and Abraham Gaikwad, a police official said.
Also Read:Orthopedician booked after female patient attendant alleges sexual harassment
The accused doctor works as an interventional cardiologist in a private hospital near Panaji, he said.
“As per the probe conducted so far, the main accused in the case, Dr Mundhekar, started abusing his fellow customer and even broke the table of the restaurant located in Old Goa village,” the official added.
The police did not specify the motive behind the assault.
Based on a complaint filed by the victim, the police registered a case against the four accused on the charges of trespassing, provocation, damage to property, assault and wrongful restraint.
Powered by WPeMatico
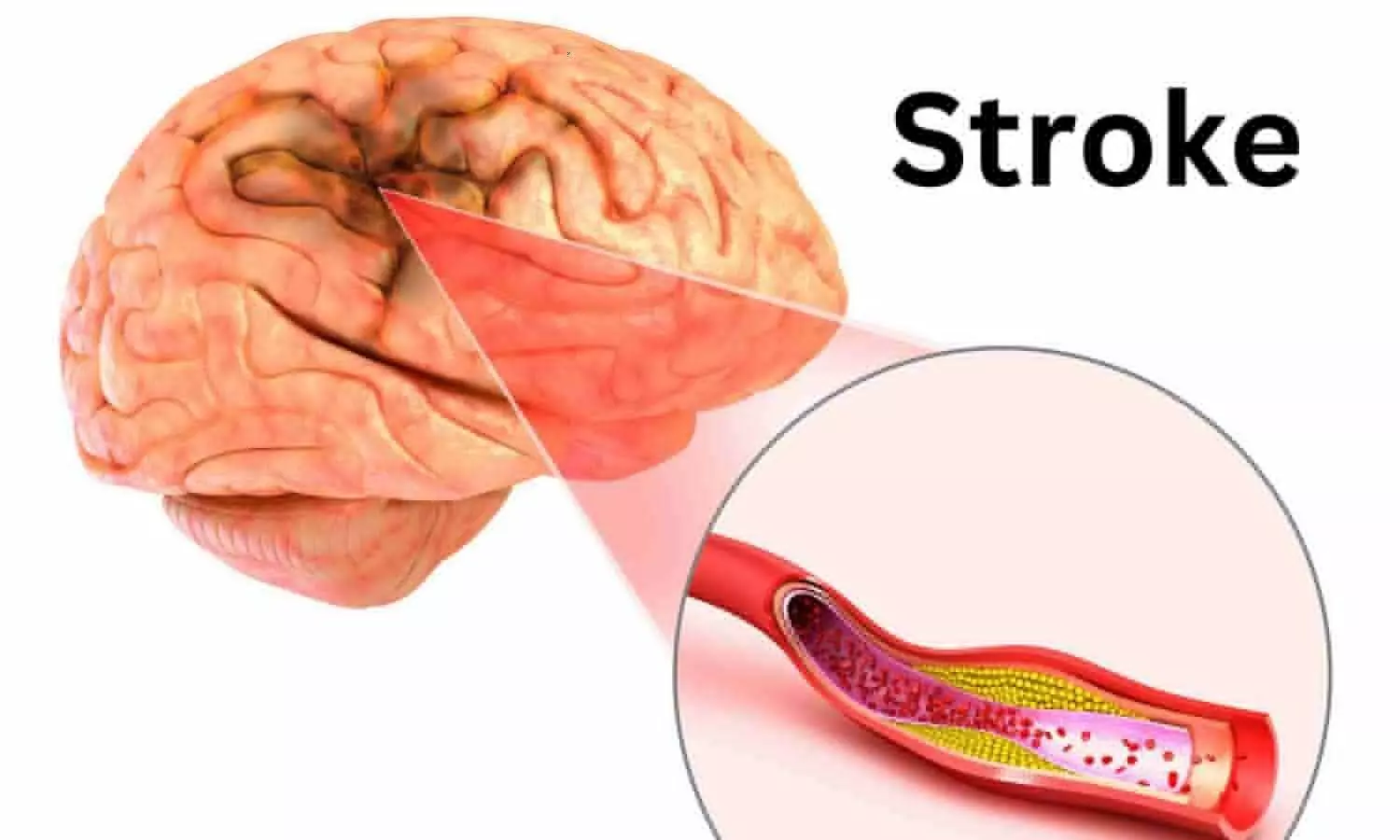
USA: Zero-degree head positioning is a safe and effective strategy to optimize blood flow to the brain until the thrombectomy can be performed, and it should be considered the standard of care for stroke patients prior to thrombectomy, a recent study has revealed.
The findings, presented as preliminary late-breaking science at the American Stroke Association’s International Stroke Conference 2024, suggest that gravitational force can play an important role in improving blood flow temporarily while patients are waiting for surgery. The meeting, held in person in Phoenix, Feb. 7 – 9, 2024, is a world premier meeting for researchers and clinicians dedicated to the science of stroke and brain health.
According to the study, positioning patients with large vessel ischemic (clot-caused) stroke with their heads flat (0-degrees) before surgery to remove the blood clot resulted in significant improvements in neurological function, compared to patients whose heads were elevated (at a 30-degree angle)..
Large vessel occlusion is a type of ischemic stroke involving blockage of a major artery in the brain. A surgical procedure called thrombectomy removes the blood clot to restore blood flow and reduce the risk of death or permanent injury to the brain including a potential loss of neurological function.
“Many thrombectomy patients have delays until the procedure can be started, whether due to slow internal hospital processes, multiple patients arriving at the same time or if the patient needs to be transferred to another hospital,” said lead study researcher Anne W. Alexandrov, Ph.D., a professor of nursing and neurology at the University of Tennessee Health Science Center in Memphis. “Optimizing blood flow to the brain while patients are waiting for surgery, is essential to minimize the risk of neurological deficits and ultimately disability.”
Currently, hospital beds for stroke patients awaiting thrombectomy surgery are typically set with the head of the bed at a 30-degree angle, or a slight incline, Alexandrov said. However, pilot studies conducted by Alexandrov’s team have shown that when the head of the bed is flat at 0-degrees, thrombectomy patients benefit from increased gravitational blood flow through the narrowed/blocked artery and more open collateral arteries for the procedure.
In this randomized clinical trial called Zero Degree Head Positioning in Acute Large Vessel Ischemic Stroke or ZODIAC, researchers used the National Institutes of Health Stroke Scale (NIHSS)-which assesses consciousness, vision, speech, motor strength and sensory loss-to evaluate stroke patients with large vessel occlusion acute ischemic stroke. They compared if patients’ conditions remained stable or worsened depending on whether they were set with 0-degree head positioning vs. 30-degree head positioning before thrombectomy surgery.
Stroke patients’ baseline NIHSS scores were measured at 0-degrees immediately after neuroimaging, then they were randomly positioned to head positioning at either 0-degrees or 30-degrees. Patients underwent repeat NIHSS scoring every 10 minutes until the thrombectomy was performed, with a final NIHSS score assessed immediately before they were positioned on the surgical table.
An interim analysis found that 0-degree head positioning before thrombectomy surgery resulted in greater stability and/or clinical improvement prior to surgery based on repeated NIHSS scores in stroke patients compared to patients with 30-degree head positioning.
The investigators also explored whether there would be differences in the NIHSS score at 24 hours following surgery and at 7 days or discharge (whichever came first), however, they didn’t expect to find a difference because thrombectomy itself dramatically improves patient outcomes. They were surprised to find that at both 24 hours after surgery and at 7 days after discharge, the 0-degree-head-position patients had less neurological deficits on the NIHSS compared to patients with head-positioning at a 30-degree incline before surgery.
“By three months following surgery, there was no difference in outcomes for patients in either group, however, it’s exciting to see that we were able to discharge patients from the hospital with less disability requiring rehabilitation,” Alexandrov said.
Due to the efficacy of 0-degree head positioning for stroke patients awaiting thrombectomy, the study’s Data and Safety Monitoring Board stopped enrollment in this trial on November 1, 2023.
“Our findings suggest that gravitational force can play an important role in improving blood flow temporarily while patients are waiting for surgery,” Alexandrov said. “Zero-degree head positioning is a safe and effective strategy to optimize blood flow to the brain until the thrombectomy can be performed, and it should be considered the standard of care for stroke patients prior to thrombectomy.”
Study background and details:
Reference:
Position of stroke patient’s head before surgery may improve neurological function, American Heart Association, Meeting: ASA International Stroke Conference 2024.
Powered by WPeMatico

Canada: A recent study showed greater treatment efficacy with the interleukin-23–receptor antagonist peptide JNJ-77242113 after 16 weeks of once- or twice-daily oral administration than placebo in patients with moderate-to-severe plaque psoriasis. The findings from the FRONTIER 1, a phase 2 dose-finding trial, were published online in The New England Journal of Medicine.
“The level of reduction of psoriasis that was observed with higher doses of JNJ-77242113 at week 16 was similar in magnitude to the responses seen with several of the injectable biologics that are currently approved for psoriasis,” investigators in the FRONTIER 1 trial wrote.
Psoriasis is an immune-mediated, multisystemic, inflammatory disease that predominantly involves the skin and joints. The disease is also a risk factor for atherosclerotic cardiovascular disease. Interleukin-23 plays an important role in pathogenic T-cell activation in psoriasis.
Using monoclonal antibodies has changed the treatment of various immune-mediated inflammatory diseases, including psoriasis. However, these large proteins must be administered via injection. Many patients prefer oral treatments over injections, and injections are especially problematic among children and among patients with a fear of needles. Thus, there is a need for efficacious targeted therapies that can be administered orally.
JNJ-77242113 is a novel, orally administered interleukin-23–receptor antagonist peptide selectively blocks interleukin-23 signalling and downstream cytokine production. Robert Bissonnette, University of Toronto, Toronto, Canada, and colleagues report the results of FRONTIER 1, a phase 2 trial of JNJ-77242113 in patients with moderate-to-severe plaque psoriasis.
In the trial, 255 patients with moderate-to-severe plaque psoriasis were randomly assigned to receive JNJ-77242113 at a dose of 25 mg once daily, 25 mg twice daily, 50 mg once daily, 100 mg once daily, or 100 mg twice daily or placebo for 16 weeks. The study’s primary endpoint was a reduction from a baseline of at least 75% in the Psoriasis Area and Severity Index (PASI) score (PASI 75 response). PASI scores range from 0 to 72, with higher scores implying greater extent or severity of psoriasis) at week 16.
The mean PASI score at baseline was 19.1. The mean psoriasis duration was 18.2 years, and 78% of the patients across all the trial groups had previously received systemic treatments.
The researchers reported the following findings:
“In patients with moderate-to-severe plaque psoriasis, JNJ-77242113 showed a dose-response relationship and greater efficacy than placebo, as measured by the PASI 75 response at week 16,” the researchers wrote. “Overall, we found no evidence of a relationship between the JNJ-77242113 dose and the incidence of adverse events.”
Limitations include a small number of patients in each trial group and the short duration of treatment. In addition, no corrections were made for multiplicity, so the researchers could not infer definitive effects of JNJ-77242113 for particular dose groups or secondary endpoints.
Reference:
Bissonnette R, Pinter A, Ferris LK, Gerdes S, Rich P, Vender R, Miller M, Shen YK, Kannan A, Li S, DeKlotz C, Papp K. An Oral Interleukin-23-Receptor Antagonist Peptide for Plaque Psoriasis. N Engl J Med. 2024 Feb 8;390(6):510-521. doi: 10.1056/NEJMoa2308713. PMID: 38324484.
Powered by WPeMatico

Recently published study aimed to assess the feasibility and safety of three-port laparoscopic cholecystectomy as an alternative to the conventional four-port approach. The study involved a prospective observational analysis of 102 patients who underwent the three-port approach, evaluating parameters such as age, sex, intra-operative difficulties, outcomes, and the need for conversion to four-port laparoscopic cholecystectomy. Modifications in the technique included the use of a pre-emptive analgesia and specific port placements. The study found that the mean operative time was 52.68 minutes, with difficulty encountered in 18.6% of cases due to various factors such as pericholecystic adhesions and mucocele of the gallbladder. The postoperative pain was minimal, with a mean visual analog scale score of 1.22, and the mean postoperative hospital stay was 1.08 days. Only 2.9% of cases needed conversion to four-port cholecystectomy for safety reasons. The study concluded that three-port laparoscopic cholecystectomy is a feasible and safe alternative, especially in difficult cases such as post-endoscopic retrograde cholangiopancreatography and mucocele of the gallbladder. The researchers emphasized that the reduced number of ports, pre-emptive analgesia, and improved cosmesis make this approach a viable option in the treatment of gallstone disease. However, they acknowledged the need for further comparative studies to establish its safety and feasibility. The study was conducted with approval from the institutional ethics committee, and the authors declared no conflicts of interest.
Reference –
Chatterjee A, Kumar R, Chattoraj A (January 13, 2024) Three-Port Laparoscopic Cholecystectomy as a Safe and Feasible Alternative to the Conventional Four-Port Laparoscopic Cholecystectomy. Cureus 16(1): e52196. doi:10.7759/cureus.52196
Powered by WPeMatico
