Lupin unveils first generic version of Oracea in US

Mumbai: Global pharma major Lupin Limited has announced the
launch of first generic version of Oracea (Doxycycline Capsules, 40 mg), in the United States, after
having received an approval from the United States Food and Drug Administration (U.S. FDA).
Read also: Lupin gets USFDA nod for generic equivalent of Oracea Capsules
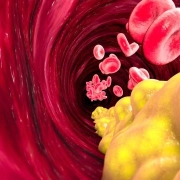
Doxycycline Capsules, 40 mg is indicated for the treatment of only inflammatory lesions (papules and
pustules) of rosacea in adult patients.
Rosacea is a chronic skin condition characterized by facial redness, visible blood vessels, and sometimes small, red, pus-filled bumps. It typically affects the central part of the face and can also involve eye irritation. While the exact cause is unknown, factors like genetics, blood vessel abnormalities, and certain bacteria may contribute.
Doxycycline Capsules had estimated annual sales of USD 128 million in the U.S. (IQVIA MAT February
2024).
Read also: Lupin bags USFDA nod for Eslicarbazepine Acetate Tablets for partial-onset seizures
Lupin is an innovation-led transnational pharmaceutical company headquartered in Mumbai, India. The
Company develops and commercializes a wide range of branded and generic formulations, biotechnology
products, and APIs in over 100 markets in the U.S., India, South Africa, and across the Asia Pacific (APAC), Latin
America (LATAM), Europe, and Middle East regions.
The Company specializes in the cardiovascular, anti-diabetic, and respiratory segments and has
a significant presence in the anti-infective, gastro-intestinal (GI), central nervous system (CNS), and women’s
health areas. The company
invested 7.9% of its revenue in research and development in FY23.
Lupin has 15 manufacturing sites, 7 research centers.
Read also: Lupin names Dr Ranjana Pathak as Chief Quality Officer
Powered by WPeMatico